Strengthen primary healthcare governance
While the public healthcare system has a strong and formal accountability system and a system is in place to hold private healthcare service providers accountable to their customers, it is necessary that we maintain the standard and quality control of the service sector as a whole. In particular, there is a need for standardisation and assurance of the quality of PHC services across public and private providers to ensure that the whole PHC system is driving towards the Government’s overall PHC policy and delivering the intended health outcomes. It is also necessary to set up an overarching governance structure to steer and enhance cross-sectoral and inter-organisational co-ordination among PHC services provided by public and private healthcare service providers at the community level. Enhancement of performance monitoring tools, and improvement on standardisation and transparency in the services across the public sector and the private sector, where PHC services take place, are some of the key issues to be addressed. With the participation of well-managed private PHC providers in the PHC system, we envisage to see improvements in the quality of health for individuals and the population as a whole.

Health system governance is the cornerstone for creating a desirable and balanced healthcare system for delivering the intended health outcomes in the healthcare system. According to the WHO, leadership and governance in building a health system is essential in ensuring that strategic policy frameworks exist and are combined with effective oversight, coalition-building, regulation, attention to system design and accountability [18].
Healthcare Governance in Hong Kong
Health Bureau (HHB) is the Government Bureau overseeing overall health system policies and responsible for the governance of Hong Kong’s healthcare system, oversight of public health and access to ensure care for all citizens. It has assumed the role of the overall commissioner of public health services through the annual budgetary and resource allocation exercise. The Government has been monitoring the operation and utilisation of resources of HA and DH through various channels.
The Department of Health
Established in 1989 upon the re-organisation of the former Medical and Health Department, DH is the Government’s health adviser which performs public health functions including health promotion, disease prevention as well as regulation of drugs and healthcare facilities. With the changing health needs of the community brought about by challenges such as changes in trends of diseases, emerging and re-emerging infections, ageing population, and advances in IT and medical technology, DH has kept reviewing its structure to keep pace with the changes and meet challenges.
With increased awareness on public health in the community, there is also growing demand on DH services such as various vaccination programmes, health promotion, strategic action plans for prevention and control of non-communicable diseases (NCDs), and implementation of various public health-related subsidy schemes (e.g. Elderly Health Care Voucher (EHCV) Scheme and Colorectal Cancer Screening Programme) (see also Chapter 2 on DH’s services).
Insofar as PHC is concerned, a dedicated Primary Care Office (PCO) was set up in 2010 to support and co-ordinate the development of primary care in Hong Kong, with particular focus on co-ordinating public and private healthcare providers and other stakeholders in the implementation of population-wide policies and strategies to enhance primary care. Among other things, PCO is responsible for work relating to the development and updating of the RFs, maintenance and promoting the use of the Primary Care Directory (PCD), and promotion of the family doctor concept and/or family medicine practice. To allow better use of the expertise and resources, and enable HHB to better drive the continuous development of the PHC system in Hong Kong, the PCO has been integrated into the PHO of FHB since October 2019 (see paragraph 93 below for functions of PHO).
At present, DH is the sole/lead agency for the administration of over 20 health-related ordinances in regulating, among other things, medical and therapeutic commodities, healthcare facilities, and harmful substances, to ensure public health and safety. With new statutes being introduced to step up protection of public health, and the advances in healthcare technologies in recent years, such as introduction of advanced therapies, development of genomic medicine, and increasing complexity in healthcare delivery and public expectation, DH has been ensuring organised efforts of the regulatory units and regimes in delivering relevant health policies, capacity building and responding to rapid development of healthcare technology and international standards. DH is also responsible for establishing and maintaining network with international and overseas health regulatory authorities.
In terms of premises of private healthcare facilities (PHFs) where doctors or dentists practise, DH is implementing the Private Healthcare Facilities Ordinance (Cap 633) in phases based on types of PHFs and their risk level. Application for hospital licences and day procedure licences have commenced since July 2019 and January 2020 respectively. For clinics, application for licence and request for letter of exemption will be announced in due course. Licensees of PHFs are required to comply with the regulatory standards covering governance, staffing, equipment and facilities related to the operation of the type of facilities as set out in the relevant codes of practice. Compliance with the Ordinance are monitored by conducting inspections, surveillance on medical events and handling complaints lodged by service users against these facilities with an independent statutory body, etc.
The Hospital Authority
Established 1990, HA is an independent statutory body established under the Hospital Authority Ordinance (Cap. 113). The Ordinance includes provisions specifying that HA should use the hospital resources efficiently to provide hospital services of the highest possible standard with the resources obtainable.
HA provides the public with a wide range of curative and rehabilitative services through its hospitals, specialist out-patient clinics (SOPCs), general out-patient clinics (GOPCs) and community outreach teams. HA is accountable to the Government through performance and quality targets and service indicators reporting to HHB, which funds HA and its services. It also provides stewardship on the number of PHC services under its umbrella, such as GOPCs and other programmes as outlined in Chapter 2.
Primary Healthcare Office
As mentioned in Chapter 2, the Government is committed to enhancing district-based PHC services in order to effectively change the current focus of healthcare services on treatment to alleviate the pressure on public hospitals by setting up DHCs in 18 districts progressively. Against this backdrop, the PHO was established under the then Food and Health Bureau on 1 March 2019 to oversee and steer the development of PHC services at the bureau level. PHO’s initial focus was on the development of DHCs as a new model to cater for the needs and characteristics of the districts and enhance public awareness of healthy living, disease prevention and self-management of health. It has since then been tasked to spearhead the overall review and future development of PHC services.
Table 3.1
- To develop District Health Centres on a district-based and new model which leverages on public-private partnership and medical-social collaboration in providing primary healthcare service
- To enhance multidisciplinary, cross-sectoral and inter-organisational co-ordination in primary healthcare
- To develop, update and promulgate the reference frameworks for primary care setting
- To maintain and promote the use of the Primary Care Directory
- To promote primary healthcare, the family doctor concept and family medicine practice
Standard Setting for Primary Healthcare Services
Primary Care Directory
In 2010, the Government published the "Primary Care Development in Hong Kong: Strategy Document" (the Strategy Document) setting out the major strategies and pathways of action for improving the delivery of PHC services in Hong Kong (see also Appendix C). The establishment of the PCD was one of the major initiatives for the development of better primary care services in Hong Kong as laid down in the Strategy Document. The PCD is a web-based electronic database containing practice information and professional qualification of primary care providers in the community, which aims to:
- provide the public and primary care providers an easily accessible electronic database containing practice-based information of primary care professionals of various disciplines in the community; and
- facilitate co-ordination among different primary care providers functioning as multi-disciplinary teams to provide more comprehensive primary care services.
Currently, three sub-directories (medical practitioners, dentists and practising Chinese medicine practitioners (CMPs)) have been established under the PCD. PCD accepts enrollment from all registered practitioners of the three practices who are committed to providing directly accessible, comprehensive, continuing, co-ordinated and person-centred primary care services regardless of their discipline and practice focus. As at August 2022, there were 2 630 doctors, 228 dentists and 1 729 CMPs on the PCD.
In order to maintain their listings on the PCD, enrollees are required to comply with certain conditions for continuous medical education and development so as to encourage professional development and provide assurance to their quality of primary care services. Apart from continuous commitment to providing primary care services, an enrollee would be required to renew their Continuing Medical Education (CME) (applicable for medical practitioners) or Continuing Professional Development (CPD) (applicable for dentists) Certificate under each CME/CPD cycle. CMPs are also required to participate in the Continuing Education in CM for renewal of their practising certificates. The conditions for maintenance of listing in the PCD are summarised in Table 3.2.
As an incentive for the enrolment and enhancement of the quality of service provision, it has been a prerequisite for medical practitioners to be enrolled into the PCD in order to join certain government-subsidised healthcare initiatives, such as the Vaccination Subsidy Scheme (VSS) and participation in the DHC network.
Table3.2
Conditions for Maintenance of Listing in the Primary Care Directory
All
- An enrolled healthcare provider shall continuously provide directly accessible, comprehensive, continuing and coordinated person-centred primary care services

Registered Medical Practitioners
- An enrolled registered medical practitioner who is not taking Continuing Medical Education (CME) Programme for specialists shall participate in the “CME Programme for Practising Doctors who are not taking CME Programme for Specialists” approved by the Medical Council of Hong Kong (MCHK) and shall accumulate the required points for obtaining a yearly CME Certificate issued by the MCHK or for becoming qualified to quote the title “CME-Certified” as approved by MCHK after the end of each CME-cycle.
- An enrolled registered medical practitioner who is a specialist included in the Specialist Register of the MCHK shall participate in and comply with the CME requirements relevant to his/her specialty as may be determined by the Hong Kong Academy of Medicine (HKAM).

Registered Dentist
- An enrolled registered dentist who is not taking Continuing Professional Development (CPD) Programme for specialists shall participate in the “CPD Programme for Practising Dentists” approved by the Dental Council of Hong Kong (DCHK) and shall accumulate the required points for becoming eligible for the issue of a CPD Certificate by DCHK after the end of each CPD-cycle.
- An enrolled registered dentist who is a specialist included in the Specialist Register of the DCHK shall participate in and comply with the CPD requirements relevant to his/her speciality as may be determined by the HKAM.

Registered Chinese Medicine Practitioners (CMPs) / CMPs with limited registration / Listed CMPs
- As per the prevailing legal requirements, registered CMPs shall participate in the Continuing Education in CM approved by the Chinese Medicine Council of Hong Kong and shall accumulate the required points for becoming eligible for the renewal of the practising certificate, which is also a requirement for enrolment in PCD.
- An enrolled CMP with limited registration or listed CMP shall have records of participating in continuing education in CM.
Reference Frameworks
The development of RFs was another major initiative promulgated in the Strategy Document which aims to guide and co-ordinate efforts of healthcare professionals across different sectors in Hong Kong for the provision of continuing, comprehensive and evidence-based care in the community; empower patients and their carers; and raise the public’s awareness on the importance of preventing and properly managing the major chronic diseases.
As in end-July 2022, four RFs comprising core documents and modules on topics about preventive care and disease management have been published (see Table 3.3). Of these, the RFs on HT, DM form an integral part of the secondary and tertiary prevention service protocol in the DHC, while the RF for older adults provides common reference for the Elderly Health Service under DH and the DHC’s fall prevention programme. In addition, the modules under the RF for children have been adopted in parent education under MCHCs.
Table 3.3
Topics currently Covered by Reference Frameworks

Diabetes Care for Adults
- Core Document
- Module 1 – Framework for Population Approach in the Prevention and Control of Diabetes across the Life Course
- Module 2 – Early Identification of People with Diabetes
- Module 3 – Dietary Intervention for People with Diabetes
- Module 4 – Recommending Exercise to People with Diabetes
- Module 5 – Glucose Control and Monitoring
- Module 6 – Drug Treatment for Hyperglycaemia
- Module 7 – Drug Treatment in Type 2 Diabetic Patients with Hypertension
- Module 8 – Lipid Management in Diabetic Patient
- Module 9 – Diabetic Kidney Disease
- Module 10 – Diabetic Eye Disease
- Module 11 – Diabetic Foot Problems
- Module on Smoking Cessation in Primary Care Settings
Hypertension Care for Adults
- Core Document
- Module 1 – Framework for Population Approach in the Prevention and Control of Hypertension across the Life Course
- Module 2 – Blood Pressure Measurement
- Module 3 – Secondary Hypertension
- Module 4 – Evaluation for All Newly Diagnosed Hypertensive Patients
- Module 5 – Dietary Intervention
- Module 6 – Exercise Recommendations to People with Hypertension
- Module 7 – Drug Treatment for People with Hypertension
- Module 8 – Annual Assessment
- Module 9 - Lipid Management in Hypertensive Patients
- Module on Smoking Cessation in Primary Care Settings

Preventive Care for Children
- Core Document
- Module on Immunisation
- Module on Development
- Module on Childhood Injury Prevention
- Module on Physical Growth
- Module on Parent Empowerment – Booklet on Child Care Tips

Preventive Care for Older Adults
- Core Document
- Module on Health Assessment
- Module on Falls in Elderly
- Module on Dental Health Care for Older Persons
- Module on Visual Impairment
- Module on Cognitive Impairment
- Module on Common Mental Health Problems in Older Adults
The Challenges
An ageing population coupled with the COVID-19 epidemic has posed tremendous challenges to the public healthcare system. To safeguard public health and strengthen the provision of services, the Food and Health Bureau was revamped as the Health Bureau on 1 July 2022 which is dedicated to medical and health policies. HHB will press ahead with a host of priority initiatives, one of which being the implementation of the Blueprint.
However, as seen from the above, the existing health governance structure has not placed enough emphasis on PHC. The health policy and decision making process has been fragmented without putting PHC at the centre of its policy focus. A holistic approach at the policy level is required in addressing the systemic imbalances between PHC and secondary/tertiary healthcare in terms of policymaking, financing, manpower, regulation, and outcome monitoring. A co-ordinated approach at the implementation level is also required to ensure commitment to drive institutional changes and enhance cross-sectoral and inter-organisational co-ordination among PHC services in an integrated manner.
At the same time, as we have again reiterated the importance of utilising the potential of the private healthcare sector, it is necessary that we maintain the standard and quality control of the PHC service sector as a whole. There are yet available tools for the Government to leverage on with a view to ensuring standardisation and assurance of the quality of PHC services across public and private providers to ensure that the whole PHC system is driving towards the Government’s overall PHC policy objectives and delivering the intended health outcomes.
Our Aim
To successfully implement various recommendations in this Blueprint, systemic changes in the governance structure should be introduced to enable a vision- and mission- led decision making process involving service assessment, resource allocation and co-ordination, generating intelligence and ensuring accountability. Our aim is to demonstrate policy commitment and drive cross-sectoral and inter-organisational co-ordination among PHC services provided by public and private healthcare service providers at the community level; and enhance standardisation and assurance of the quality of PHC services across sectors to ensure that the whole PHC system is delivering the intended health outcomes.
With the above intent, we propose the following –
Recommendation 3.1
Establishment of Primary Healthcare Commission
We consider that an overarching governance structure focusing on positioning PHC as a health system priority is essential to enable a vision- and mission- led policymaking process. An overarching governance body shall also provide oversight and bring together multiple agencies and align their efforts to ensure that the health system meets its targets, goals and duties in the delivery of services.
To this end, the Government proposes to progressively transform the PHO currently under HHB into an overarching PHC governing body, the Primary Healthcare Commission, to ensure effective and efficient utilisation of resources, promote seamless care across all government-subsidised healthcare services by ensuring effective cross-institutional and cross-sectoral collaboration, enhance monitoring of performance of different PHC services, and demonstrate the Government’s commitment and support in developing a sustainable PHC system.
It is recommended that the Primary Healthcare Commission should be positioned to oversee –
- the provision of PHC services, including service planning and resource allocation through strategic purchasing supported by the newly established Strategic Purchasing Office (SPO),
- standard and protocol setting for both public and private service providers, quality assurance and monitoring of private PHC services, and
- the training of PHC professionals.
With gradual service integration as illustrated in Chapter 2, the Primary Healthcare Commission should be tasked to review the roles of different key service providers in PHC and enhance cross-sectoral and inter-organisational co-ordination. In terms of standard setting, patients requiring access to public secondary healthcare services should be subject to protocol-driven assessment at the PHC level to reduce service duplication and abuse of public secondary healthcare services (see Recommendations 3.2 and 3.3 below).
At the initial stage, the Primary Healthcare Commission would leverage on the existing manpower and structure relocated from both DH and HA to set up an executive arm for serving the dual functions of service standard setting and quality assurance, with support of a SPO in the procurement of PHC services in the private sector. It is envisaged that new legislation(s) would be required to provide the mandate and statutory powers for the Primary Healthcare Commission to implement the standards (as promulgated in Recommendations 3.2 and 3.3) on private PHC service providers other than through contract provisions. The Primary Healthcare Commission will be a change agent to facilitate cross-sector collaboration.
With the establishment of the Primary Healthcare Commission and the service integration plan as outlined in Chapter 2, the Government proposes to also realign the focuses and roles of DH and HA.
The Department of Health’s Role
Upon the establishment of the Primary Healthcare Commission, DH will maintain its public health functions and continue to serve as the Government’s public health adviser in planning the overall public health strategy over the territory and executing its regulatory and enforcement roles (including regulation of drugs, healthcare facilities, tobacco and alcohol control). In addition, the core functions of DH in formulating and implementing public health strategies will also be strengthened, as well as monitoring and facilitating the development of health technology and the research and development of drugs, so as to enhance its capability to cater for the future development of society and public health.
Under the new role delineation, some of DH’s direct PHC services would be gradually integrated into the Primary Healthcare Commission, depending on their respective service model, scale, and extent of service duplication with other service providers in the community. As a start, as the service model and scale of DHCs continue to grow and solidify, and given that there is a considerable extent of service duplication with DH, we propose certain PHC services to be gradually integrated with DH’s, such as elderly health services, woman health services, health promotion, as well as other programme-based PHC services such as cancer screening (see Chapter 2). Meanwhile, other PPP programmes, such as various subsidised vaccination and screening programmes currently administered by DH, should be considered for integration under the Primary Healthcare Commission with partnership with private healthcare practitioners as appropriate upon SPO’s review. The Primary Healthcare Commission and the newly set up SPO will recommend alternative approaches on service delivery in these areas with a view to allowing more cost-effective provision of healthcare services while maximising population health beyond the existing direct service delivery mode (see Chapter 4).
The re-organisation of DH upon establishment of the Primary Healthcare Commission will also enhance DH’s capacity to keep abreast of and respond promptly to new developments and protect Hong Kong’s public health. Focusing on public health regulatory affairs, the safety of healthcare services and products will be regulated in a more organised manner and the standard of healthcare industry is expected to be enhanced to safeguard public health. It will also enable the adoption of more co-ordinated efforts to achieve regulatory efficiency in meeting public demand and facilitating business operation.
The Hospital Authority’s Role
On the other hand, while HA currently has also provided a range of PHC services to the community, with the establishment of the Primary Healthcare Commission, HA is envisaged to focus on its provision of public hospital and related medical treatment and rehabilitation services to the public in accordance with the Hospital Authority Ordinance, whereas its PHC services (e.g. the GOPCs) should follow the policy direction from the Primary Healthcare Commission and only focus to serve as an essential safety net for the population, especially those who lack the means to pay, as elaborated under Recommendation 2.3. The budget for respective PHC services should also be separated from HA’s overall budget and put under the planning provision from the Primary Healthcare Commission.
Strategic Purchasing Office
With the establishment of the Primary Healthcare Commission which assumes the role of resource allocation, it is necessary to look into most efficient ways in delivering PHC beyond the existing model through strategic purchasing. Strategic purchasing aims to maximise healthcare system benefits through an active, evidence-based process that defines which health services to be bought from whom, how these health services should be paid for, at what rate should be paid, and the payment and incentive mechanisms.
To improve accessibility to quality health services for the general public and redress the imbalance between public and private healthcare services, the Government proposes to leverage on HA’s and DH’s existing manpower and resources to set up an SPO to oversee the development and implementation of programmes under strategic purchasing of healthcare services particularly at primary level under HHB’s policy steer. Under the Primary Healthcare Commission’s and HA’s oversight respectively, resources are to be channeled more effectively towards quality, co-ordinated and continuous PHC with an emphasis on community-based, family-centric and prevention-oriented services, reduce service duplications, gaps inefficiencies and mismatches between the public and private sectors in PHC, and ultimately bring about optimised, co-ordinated and integrated care to individuals and families to maximise their health benefits and outcomes. Insofar as PHC is concerned, while the Primary Healthcare Commission should determine the services to be provided, SPO shall be responsible to assess strategically as to how and from whom the services are to be purchased as well as the incentive mechanism and optimum payment level in order to ensure overall cost-effectiveness. Details of strategic purchasing and SPO will be discussed Chapter 4.
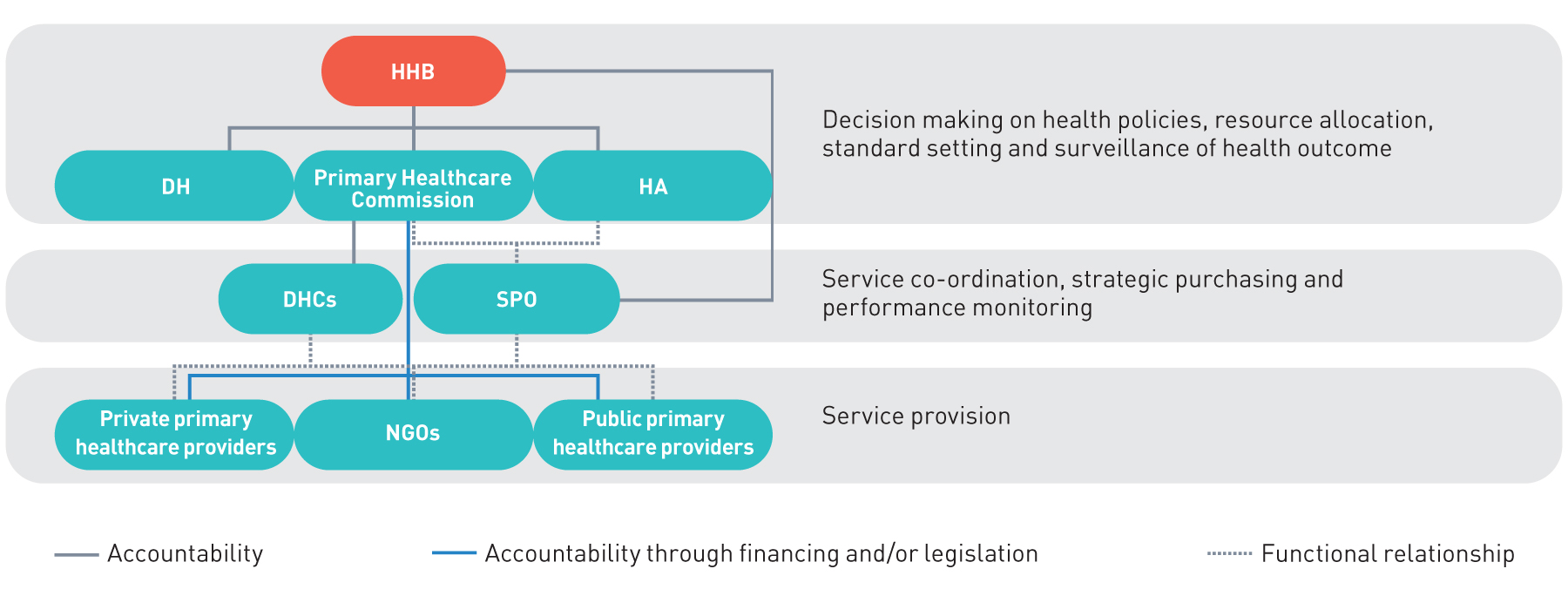
The governance structure and functional relationship between different bodies under HHB is illustrated in Figure 3.1.
Figure 3.1
The proposed healthcare system governance structure and functional relationship
Recommendation 3.2
Standardised care for healthcare professionals participating in PHC service provision
As discussed in Chapter 1, the potential of the private PHC sector should be better utilised through improved co-ordination, resource allocation and policy steer. Private healthcare resources, if utilised properly, should alleviate the pressure on the public healthcare sector and thereby support a sustainable healthcare system.
During COVID-19, the Government has tapped into private healthcare resources for a number of initiatives against the epidemic, ranging from sentinel surveillance of suspected COVID-19 cases, the territory-wide COVID-19 vaccination programme, operation of community isolation facilities, to provision of COVID-19 drugs to patients in the community. Supported by the active involvement and participation of the private sector in operating service centres or provision of service in their private clinics, the Government was able to roll out these initiatives at light speed across the territory, which allowed us to gear up quickly in the face of the unprecedented healthcare crisis. This illustrates the importance and possible scope of how we could leverage the efficiency of private resources in the context of healthcare.
Experience from many developed countries shows that sharing population-based common clinical management models and protocols among healthcare providers in different settings facilitates the co-ordination of care, strengthens management continuity, promotes evidence-based practice and improves patient care [11]. To further promote development of PHC at the community level and establish policies and standards for various PHC service providers under a co-ordinated PHC system, we propose the following improvements to the existing PCD and RFs in order to transform them into levers for standardised care and quality assurance tools.
Primary Care Register
We recommend to redefine the role of the PCD into a Primary Care Register (PCR) which could serve as a central register for all PHC professionals under one umbrella for better monitoring, co-ordination and quality assurance. To transform the PCD into the PCR, the following aspects would be addressed:
a. Strengthening the entry and maintenance requirement
Enrollment in the PCD is currently on a voluntary basis with no entry requirements except for holding registration licence and continuous medical education certificates. Also, apart from self-declaration, there is no clear definition to the primary care-related practice focus of the healthcare practitioners.
In order for the PCR to serve as a central database for better monitoring, co-ordination and quality assurance, the Government will review the entry and maintenance requirement to the PCR. We recommend to include PHC training as one of the key enrolment or maintenance requirement.
b. Developing sub-directories for pharmacists and allied health professionals
In order to facilitate co-ordination of multi-disciplinary teams to provide comprehensive PHC services, the Government will continue developing sub-directories for pharmacists and other allied health professionals. The sub-directories will focus on enhancing collaboration of multiple disciplines and quality assurance of pharmacists and allied health professionals in supporting Government PHC initiatives. The sub-directories will be shared among PHC service providers and provided to patients to facilitate their choice upon referral.
It is suggested to first develop sub-directories for PTs, OTs and pharmacists in view of their extensive involvement in PHC for various medical conditions, in particular on chronic illnesses and long-term care. Sub-directories of other healthcare professionals (e.g. optometrists, nurses, speech therapists, dietitians, and other professionals who are not subject to any statutory registration requirements) are recommended to be developed in a later phase.
c. Adoption of standard care protocol and the use of (eHealth)
All PCR participants would be subject to quality assurance as set by the Primary Healthcare Commission. Among other things, they are required to follow the RFs promulgated by the Primary Healthcare Commission for handling specific chronic diseases (see paragraphs 128 to 132). Other quality assurance measures such as review and evaluation of practice, as well as performance indicators for PHC would be explored.
In addition, the use of eHealth for documentation of patients’ records will become mandatory for healthcare providers on the PCR in order to facilitate continuity of care and allow better integration throughout the whole healthcare delivery process (see Chapter 6 for details of eHealth).
Reference Frameworks
We propose to establish the RFs as the standard care protocol in PHC services, particularly in government subsidised services, to enhance healthcare quality and facilitate multi-disciplinary care.
On top of the four RFs promulgated by the Government, covering HT, DM and preventive care for children and older adults in primary care settings (see Table 3.3), we will further develop and expand the applicability of the RFs to various disease groups with emphasis on patient empowerment and strengthening of multi-disciplinary care.
To support the future development of RFs with emphasis on patient empowerment and strengthening of multi-disciplinary care, the PHO has formed an Expert Panel on Reference Frameworks with experts of different backgrounds and specialties to advise the Government on the development, updating, promulgation and adoption of RFs in various settings. The PHO shall prioritise the development of new RFs and update existing RFs in a timely fashion having regard to the comments from the Expert Panel and international development. Table 3.4 shows some of the potential topics of new RFs which are drawn up having regard to disease prevalence and international evidence on the effectiveness of PHC intervention. The involvement of CM in the RFs will be further explored with a view to unleashing the potential advantage of CM in health management and facilitating multi-disciplinary collaboration in PHC settings (including pure CM and integrated Chinese-Western medicine approaches).
Quality assurance of PHC practitioners
Table 3.4
- common musculoskeletal problems
- woman’s health
- chronic obstructive pulmonary disease
- common mental problems
- chronic hepatitis
The Primary Healthcare Commission will be tasked to oversee the improvements on the PCR and RFs as mentioned in the above paragraph. To effectively utilise the above policy levers, the Government proposes to require all family doctors and healthcare professionals participating in PHC service provision to be enlisted on the PCR and commit to use RFs, including those enrolling in government-subsidised programmes such as the EHCV Scheme, various PHC PPP Programmes, vaccination programmes, population-wide screening programmes such as Colorectal Cancer Screening, as well as the CDCC Scheme) as mentioned in Recommendation 2.2, in order to provide quality assurance to users of PHC services, establish the “gold standard” for PHC service providers, and provide incentives for PHC professionals to adopt best practices and participate in co-ordinated care.
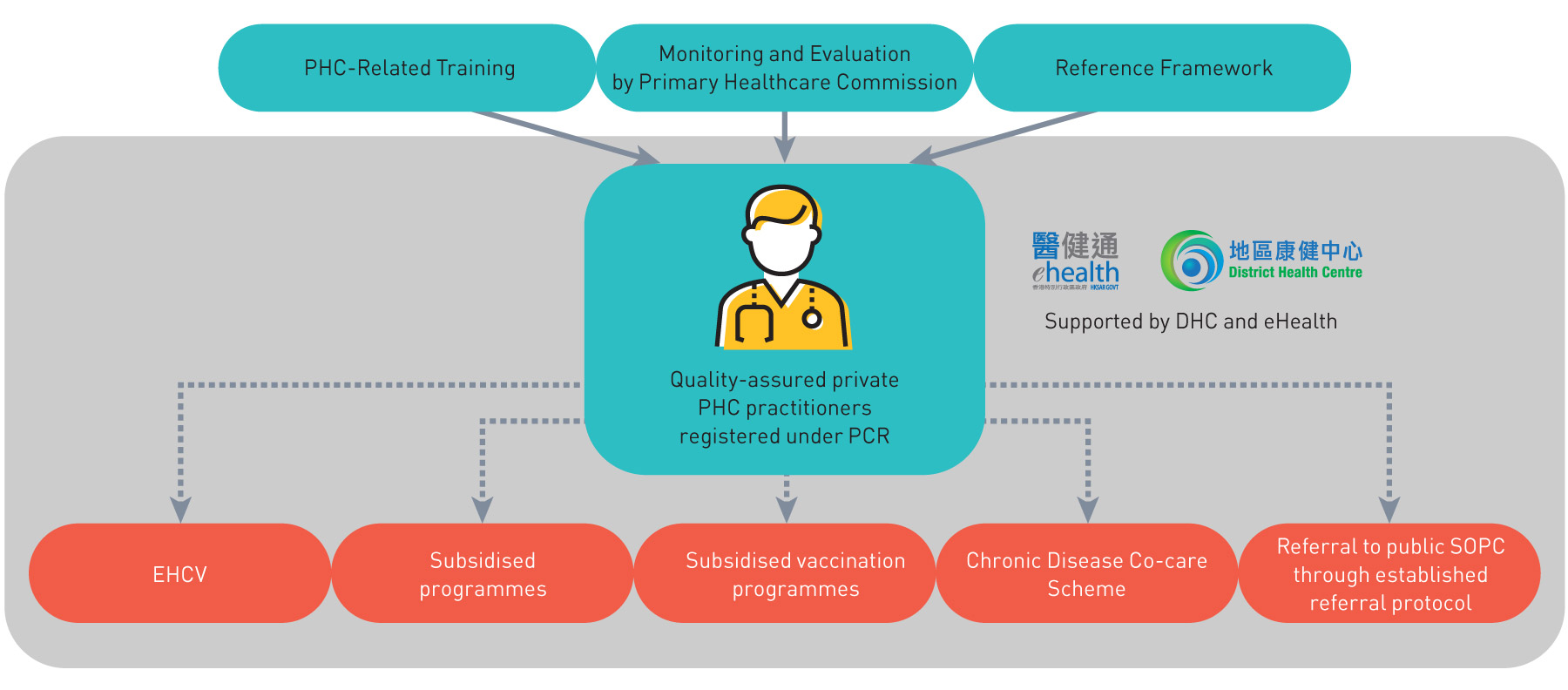
Through enrolling in PCR and compliance with the standards of RFs with legal mandate, continuous improvements in health service quality and performance of PHC practitioners and standards of PHC services is envisaged. With the extensive use of eHealth and support by DHC’s multi-disciplinary team, connection, communication and co-ordination between different healthcare providers in various settings and programmes will also be enhanced. A conceptual diagram on the governance of private PHC practitioners through various policy levers is set out in Figure 3.2.
Figure 3.2:
A conceptual diagram on the governance of private PHC practitioners through various policy levers
Recommendation 3.3
Establish an evidence-based, two-way protocol-driven primary-secondary referral mechanism
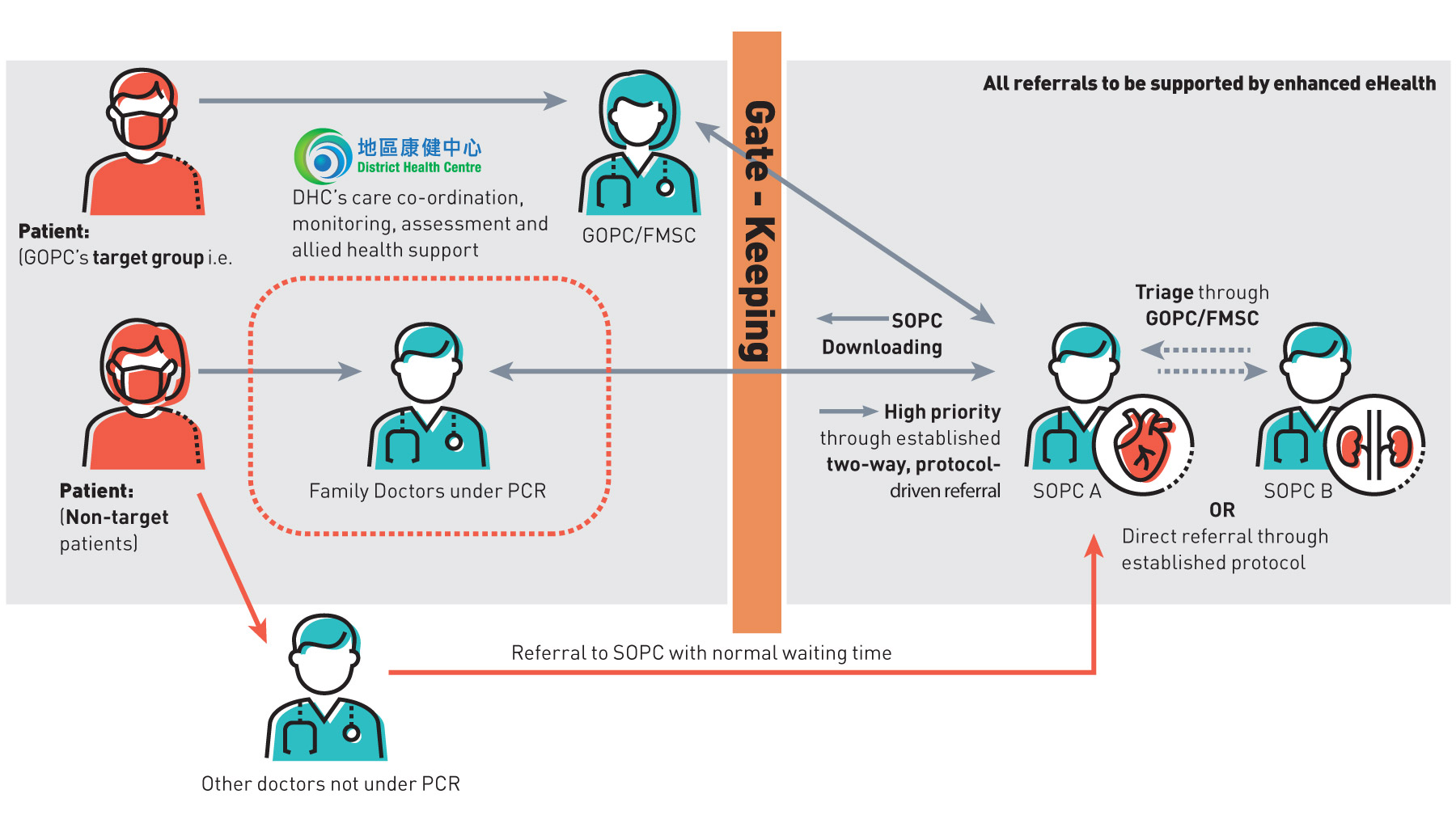
To address the problem of unclear patient pathway and multiple points of contact in the current healthcare system, GOPCs and the private PHC doctors should strengthen their role as the first contact point of the healthcare system and gate-keeper of access to secondary and tertiary care. A clear patient pathway and referral protocol are required so that the service model should be revamped to de-duplicate the functions of GOPCs and SOPCs; and for GOPCs and PHC doctors to gate-keep the access to the public secondary healthcare system.
In order to achieve the above, an evidence-based, two-way protocol-driven referral mechanism, in particular for target chronic diseases, should be established for use by both the public and private sector to ensure only those warranted cases would be uploaded to the secondary level; whereas stable cases should be downloaded back to the primary level for ongoing care.
The referral protocol between primary and secondary/tertiary care would be supported by eHealth and developed by HA through the existing referral system in the public health system, starting with target chronic diseases (i.e. hypertension and diabetes mellitus). Upon its development, we recommend to establish the primary-secondary referral mechanism between PHC service providers in both the public and private sectors with the specialist and hospital services, emphasising the effective discharge of case management and gate-keeping role of PHC service providers, allowing timely and appropriate referral of patients in serious conditions by PHC doctors to specialists and hospitals for secondary care, and allowing continuing follow-up, monitoring and disease management of patients in stable conditions by primary care doctors. In particular, the protocol shall be adopted by private PHC service providers participating in the CDCC Scheme under Recommendation 2.2 for referrals to and from the public SOPCs.
Through effective gate-keeping and triage, we envisage that the improved PHC system should be able to serve as the gate-keeper and case manager to the public secondary healthcare system with the aim of retaining most of the patients with stable condition at the primary level most of the time, and helping patients navigate each level of the healthcare system efficiently and thereby addressing the need, demand and the waiting time for SOPCs (see Figure 3.3).
In addition to the above, Hong Kong’s first Chinese medicine hospital (CMH) is targeted to commence services by phases from 2025. CMH, as a flagship CM institution leading the development of CM, will provide subsidized primary and secondary/tertiary care services to the public. The referral mechanism between CMH and relevant parties of the healthcare system (including but not limited to CM service providers) will be further explored. Moreover, mechanism that facilitate the interaction of CMPs with other healthcare professionals as well as the application of CM in PHC settings will also be considered.
Figure 3.3
A conceptual diagram on the streamlined primary-secondary referral mechanism
Chapter 3 - STRENGTHEN PRIMARY HEALTHCARE GOVERNANCE: Action Plan
3.1 Primary Healthcare Commission
To expand PHO’s establishment by introducing regional governance structure
Action: Short
To expand PHO by leveraging on the existing manpower from DH and HA
Action: Short - Medium
To establish the Primary Healthcare Commission with new legislation to provide the mandate and statutory powers for the Primary Healthcare Commission to implement the standards on private PHC service providers
Action: Short - Medium
3.2 Primary Care Directory
To develop sub-directories for pharmacists and other health professionals in the Primary Care Directory (PCD)
Action: Short - Medium
To review the enrolment or maintenance requirement for the PCD
Action: Short
To require healthcare practitioners joining designated subsidised programmes to register in PCD
Action: Short
To establish the Primary Care Register (PCR), with the support of eHealth and legal backing by relevant ordinance
Action: Medium
3.2 Reference Frameworks in Primary Care Setting
To develop and expand the applicability of the Reference Framework (RFs) to various disease groups and to explore the involvement of CM in the RFs
Action: Short - Medium - Long
To establish the RFs, with the support of eHealth backed by the Primary Healthcare Commission as the standard of care protocol for PCR healthcare practitioners
Action: Medium
3.3 Primary-secondary referral mechanism
To devise the primary-secondary referral mechanism based on the existing referral system in the public health system
Action: Short - Medium - Long
To promulgate relevant referral mechanism for the CDCC Scheme
Action: Short
To implement the referral mechanism with the support of eHealth and backing by Primary Healthcare Commission in the public and private sectors
Action: Medium

