Reinforce primary healthcare manpower
The sustained delivery of quality and adequate PHC services relies on a stable and sufficient supply of qualified PHC manpower with the necessary knowledge, skills and attitude, who embrace the concept of multi-disciplinary teamwork in PHC in the community. The training and enhancing of the role of PHC professionals is essential to ensure adequate and quality manpower supply for an effective PHC system in Hong Kong.
Our healthcare system is supported by a team of dedicated healthcare professionals. As at end of 2020, there are over 117 000 healthcare professionals from the 13 professions which are subject to statutory registration.
Table 5.1
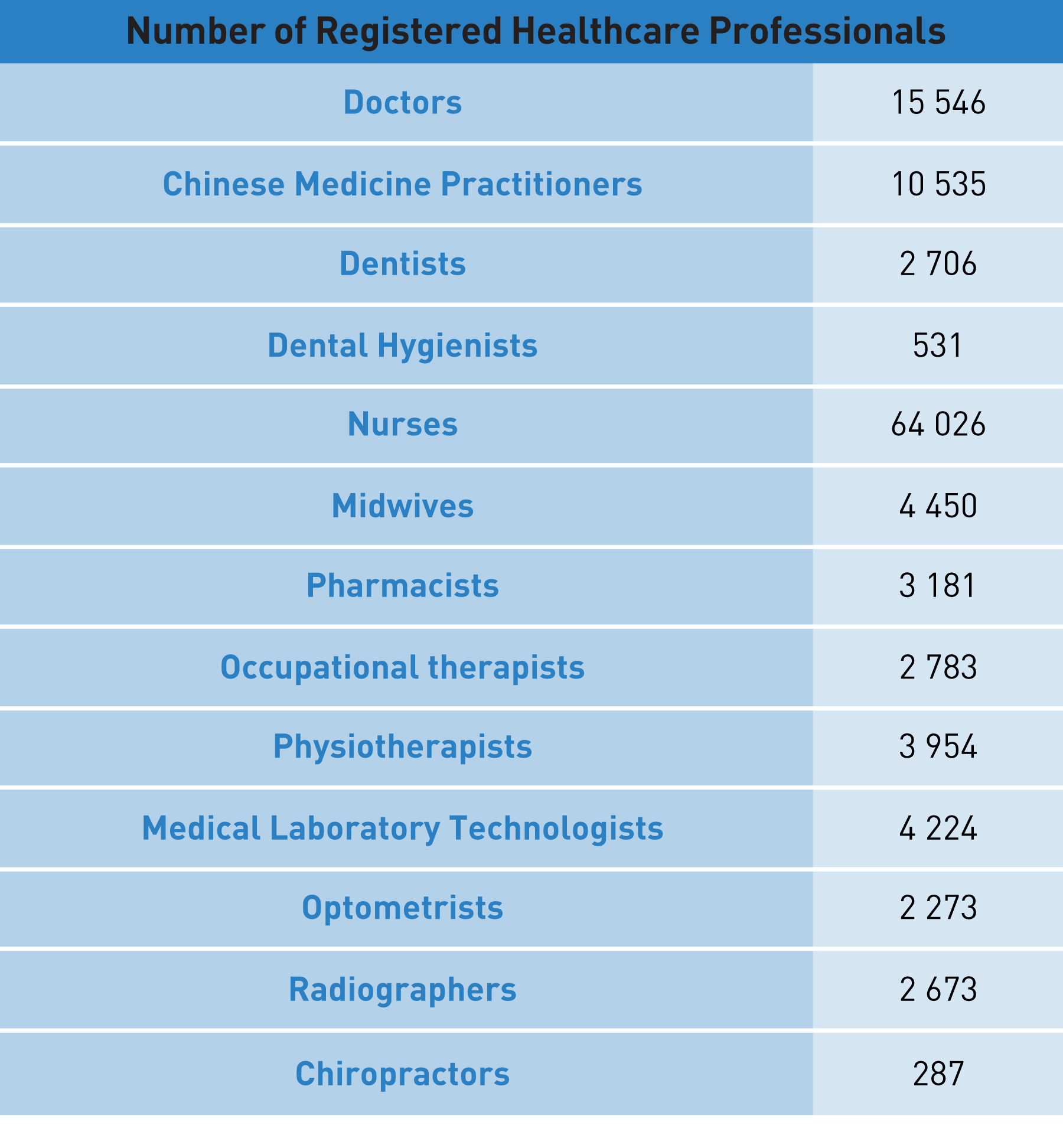
Source: Healthcare Manpower Planning and Projection by HKU
Figure 5.1:
Number of registered healthcare professionals
Source: Healthcare Manpower Planning and Projection by HKU
Healthcare Manpower Supply
The Government has been adopting a multi-pronged approach to enhance healthcare manpower. At present, local graduates from University Grants Committee (UGC)-funded programmes and self-financing programmes are the primary source of manpower supply for most of the healthcare professions, supplemented as necessary by qualified non-local ones through established mechanism in the short term. In light of an ageing population, general shortage of healthcare manpower, and expanding provision of healthcare services, the Government has further increased UGC-funded healthcare training places for doctors, nurses, pharmacists, and allied health professionals since the 2009/10 triennium.
Primary Healthcare Training
Currently, PHC elements have been embedded in the curriculum of most of the relevant undergraduate and postgraduate healthcare training programmes.
To develop an effective PHC system, we recognise the need to ensure adequate and quality supply of PHC manpower with sufficient knowledge, skills and comprehensive understanding of the multi-disciplinary PHC team and the role of each type of healthcare professionals under PHC settings including the DHC network. Training for PHC professionals is important to enable the delivery of comprehensive and sustainable PHC services under a team approach.
To facilitate the territory-wide rollout of DHCs, PHO has been working with the Hong Kong College of Family Physicians (HKCFP), the College of Ophthalmologists of Hong Kong (COHK), the Hong Kong Academy of Nursing (HKAN), and the Hong Kong Polytechnic University (PolyU) to develop relevant PHC training courses for enhancing the skills and encouraging healthcare professionals to play a more active role in the development of PHC for Hong Kong. With an emphasis on medical-social collaboration, PHO has also worked with The Hong Kong Council of Social Service on a certificate course in “Primary Healthcare for Social Workers”. As an incentive for enrollment, the Government reimburses 25% of the course fee for participants who have successfully completed the designated training course. A list of those training courses can be found in Table 5.2.
Table 5.2
Primary Healthcare Training Courses Currently Offered for Professionals

Medical Practitioner
The Hong Kong College of Family Physicians (HKCFP)
- Certificate Course in Essential Family Medicine
- Diploma Course in Family Medicine
HKCFP and the College of Ophthalmologists of Hong Kong (COHK)
- Certificate Course in Ophthalmology for Primary Care Doctors

Nurse
The Hong Kong Academy of Nursing (HKAN)
- Post-registration Certificate Course in Primary Health Care Nursing (DHC Module)

Physiotherapist
The Hong Kong Polytechnic University (PolyU), The Spastics Association of Hong Kong (SAHK) Institute of Rehabilitation Practice and the Hong Kong Physiotherapy Association
- Professional Certificate in Primary Healthcare in Community Care Context for Physiotherapy

Occupational Therapist
PolyU and the Hong Kong Occupational Therapy Association (HKOTA)
- Professional Certificate in Primary Healthcare for Occupational Therapy

Social Worker
The Hong Kong Council of Social Service
- Certificate in Primary Healthcare for Social Workers
The Challenges
As recommended in the Report of the Strategic Review on Healthcare Manpower Planning and Professional Development published in 2017, the Government conducts a healthcare manpower projection exercise every three years to update the supply and demand figures of different healthcare professionals, in step with the triennial planning cycle of the UGC. The last round of the manpower projection exercise was conducted in 2020 and the results were announced in March 2021. According to the latest manpower projection published in March 2021, as compared with the results in 2017, the shortage of doctors, nurses, dentists, physiotherapists (PTs), medical laboratory technologists, optometrists and radiographers persists, with gaps further widened for the shortage of doctors and nurses in the short and medium-term [23]. In particular, the numbers of doctors and nurses per 1 000 population are fewer in Hong Kong as compared with other high income economies [24, 25].
Against the backdrop of the general shortage of healthcare manpower in Hong Kong, the challenge of attracting and retaining healthcare professionals, especially medical practitioners, in the practice of PHC is even more acute in view of the comparatively stable career path in the secondary and tertiary care sectors which is largely dominated by the public healthcare system.
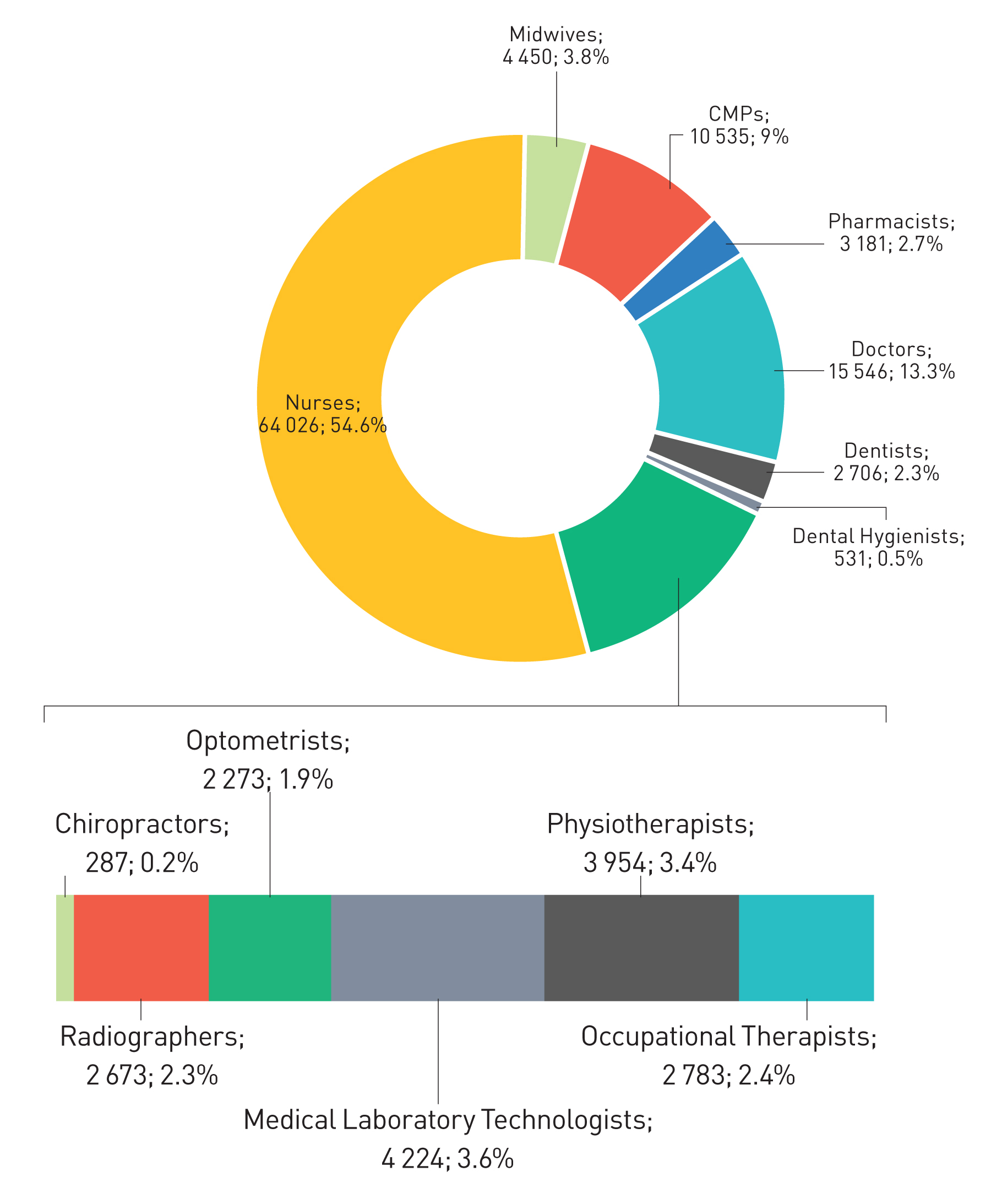
Figure 5.2:
Distribution of ealthcare professionals in the private sector and public sector
Source: The DH's Health Manpower Survey (consolidated data from 2014 to 2018)
Our Aim
Sufficient healthcare manpower is a must for the development of an effective PHC system. Our aim is to ensure adequate and steady supply of PHC manpower with the necessary knowledge, skills and attitude, embracing the concept of multi-disciplinary teamwork in PHC, so as to cope with an ageing population. We also aim to progressively enhance the role of CMPs, community pharmacists as well as other PHC professionals in the delivery of PHC services, through undergraduate and postgraduate education and clinical practice in PHC, and professional-driven and evidence-based development of care models and protocols under the aegis of the Primary Healthcare Commission with necessary resource allocation and referral pathways as part of the co-ordinated and continuous PHC at community level.
To strengthen the PHC workforce and professional training for PHC professionals against the above backdrop, we propose the following –
Recommendation 5.1
Ensure adequate supply of primary healthcare-related professionals
The Government has been adopting a multi-pronged approach to enhance healthcare manpower with a view to supporting the development of various healthcare services. Based on projections, the Government has further increased the number of training places for medical students from 530 to 590 per cohort in the 2022/23 to 2024/25 triennium. The Government has also invited self-financing institutions to provide a total of 180 additional training places for nursing students in the 2022/23 academic year.
To ensure sustainable supply of PHC manpower, especially against the backdrop of a general shortage of healthcare manpower in Hong Kong, the Government will adopt the following strategies going forward –
- in the short run, the Government will increase the number of UGC-funded healthcare training places in the coming triennium cycles and subsidise designated full-time locally accredited self-financing undergraduate and postgraduate programmes;
- it will invite the relevant professional Boards and Councils of healthcare professionals to consider increasing the weighting of PHC in their accreditation and placement programme during the regular review of the existing undergraduate and postgraduate curriculum; and
- the Government will also review the manpower projection model and formulate strategies to systematically project the demand for PHC professionals taking into account healthcare demands of the population as a whole, the recommendations in the Blueprint, and provision of PHC services in both the public and private sectors, with a view to ensuring a sufficient supply of PHC professionals through provision of subsidised local training places as well as attraction of non-locally trained professionals.
Doctors
Among all practices, family doctors play a pivotal role in providing comprehensive, continuous, whole person care to the citizens, from prevention to treatment of diseases. Family doctors also represent an important node in the PHC system, not only by providing health assessments and identification of risks to facilitate early intervention and performing diagnosis, but also by offering comprehensive, continuing and holistic care of individual patients in collaboration with other healthcare professionals under the concept of multi-disciplinary care.
To alleviate the shortage of doctors in the public healthcare system, the Government secured the passage of relevant legislative amendments in October 2021 to create a new pathway, namely special registration, for qualified non-locally trained doctors to obtain full registration in Hong Kong, subject to certain requirements or criteria being met. In accordance with the amended Medical Registration Ordinance (Cap. 161), the Registrar of Medical Practitioners (i.e. the Director of Health) announced in April 2022 and June 2022 the first two batches of a total of 50 medical qualifications recognised by the Special Registration Committee.
According to the 2018 Health Manpower Survey conducted by DH, among the active doctors enumerated who were trained in one field of specialist training, only about 8% were trained as family medicine specialist [26]. Whilst a family doctor in Hong Kong can be a GP, a family medicine specialist or any other specialist, the Government will continue to strengthen and enhance resources to enable PHC doctors to receive family medicine-related training. In addition, with the new registration pathway stated above, the Government looks forward to attracting qualified non-locally trained PHC professionals, especially family doctors, to practise in Hong Kong.
Other healthcare professionals
For healthcare professionals such as nurses and allied health professionals, apart from the usual undergraduate programmes, the Government will support some healthcare-related taught postgraduate programmes from the 2023/24 academic year onwards to facilitate first degree-holders from non-healthcare disciplines to step into the healthcare sector and become healthcare professionals. Furthermore, we will provide an additional 500 designated places under the Study Subsidy Scheme for Designated Professions/Sectors for healthcare-related self-financing undergraduate programmes per cohort starting from the 2023/24 academic year to enable more eligible students to pursue their studies in healthcare-related disciplines. The Government is working out the details of the above-mentioned initiatives with the UGC-funded universities and the self-financing institutions, and will encourage them to train more healthcare professionals required for the public healthcare system.
Recommendation 5.2
Enhance primary healthcare-related training for healthcare professionals and promotion of a multi-disciplinary approach
Multi-disciplinary care is one of the focuses in delivering PHC services and management of chronic diseases. Healthcare professionals, including doctors, CMPs, dentists, nurses, different allied health professionals such as PTs, occupational therapists (OTs), speech therapists, podiatrists, dietitians, as well as social workers, all have their distinctive roles in achieving co-ordinated, family-centric and community-based PHC services. The Government sees the need to further develop and unleash the potential of these professionals in supporting the development of PHC in Hong Kong.
To address the training and development needs of PHC professionals, the Government proposes to enhance PHC training for all PHC service providers and to set training requirements under the PCR, to facilitate healthcare related professionals in both the public and private sectors to play a more active role in the development of PHC under a team approach and operate in a co-ordinated fashion as part and parcel of the district-based community health system.
To further strengthen the training on PHC, as stated in Recommendation 5.1, the Government have invited the Boards and Councils of various healthcare professions to review and consider how to increase the weighting of PHC elements in the context of their regular review of accredited training programmes. As for practicing professionals (regardless of working in the PHC sector or not), building on the development in paragraph 176, the Government shall continue to work with different academic/training institutions to provide PHC related training for professional members of the multi-disciplinary PHC team. We will continue to evaluate and refine the training courses and explore the opportunity to work with different academic/training institutions to design PHC training for different healthcare and related professionals in support of PHC development in Hong Kong.
Upon the establishment of the Primary Healthcare Commission, the Government also proposes to look into the co-ordination of training in different healthcare settings and developing a structured rotation system to facilitate the training of family doctors and other PHC professionals in different training settings in a co-ordinated manner. We will also look into ways to construct a clearer professional development and career pathway and relevant incentives to attract healthcare professionals in pursuing a career in PHC.
Recommendation 5.3
Enhance the role of Chinese Medicine Practitioners and Chinese medicine in the primary healthcare services
Being an integral part of Hong Kong’s healthcare system, CM plays an important role in the area of PHC to safeguard public health and well-being in concerted efforts with the other healthcare professions. In fact, the Government has all along been promoting the development of CM in Hong Kong, and reaffirmed in the 2018 Policy Address the positioning of CM in the development of healthcare services in Hong Kong. Specifically, the Government subsidises a series of defined CM services to provide a comprehensive network for the delivery of government-subsidised CM services. Besides, in view of the relatively adequate and stable supply of CMP manpower in Hong Kong and the fact that over 90% of CM services are provided in the private market, the role of CM in PHC setting could be further explored with a view to fully utilising and unleashing the potential of the resources concentrated in the CM private market.
During the COVID-19 pandemic, with the support and facilitation of HHB, in relation to PHC services, HA launched a special CM out-patient programme to provide CM general consultation out-patient rehabilitation services to COVID-19 infected patients who have been discharged from public hospitals and persons who have completed isolation, through the 18 CMCTRs. Furthermore, CMPs in private practice also play an instrumental role in safeguarding public health during the pandemic by providing professional CM support and treatment to the public and taking their own initiatives to offer telemedicine and related services.
Considering the need to mobilise the resources of CM sector in the private market in our fight against the COVID-19 pandemic, HHB also rolled out a special support scheme through the Chinese Medicine Development Fund (CMDF) to subsidise CMPs to provide free telemedicine service and delivery service of CM to those infected with COVID-19 and staying at home. Recently, another special programme, which is also funded by CMDF, has been launched to provide free CM rehabilitation consultations and treatments to citizens that suffered from sequelae of COVID-19.
Having regard to the severe impact of the fifth wave of the epidemic on elderly persons at residential care homes for the elderly (RCHEs), under the support by HHB, the HA speedily took the lead in mobilising CMPs to participate in a special CM programme through community CM service providers such as universities, CM sector, CMP academic associations and NGOs, etc., to provide telemedicine or outreach CM services to infected residents and staff of RCHEs. The service concerned has subsequently been further expanded to cover CM rehabilitation consultations, such that recovered RCHE residents can receive treatment at the RCHE without travelling.
The experience of using CM in the fight against COVID-19 has clearly demonstrated the strengths and advantages of CM in PHC setting and beyond. In the long term, as CM constitutes an integral part of Hong Kong’s healthcare system, with a view to better leveraging on the strengths and advantages of CM, the Government will continue to strengthen the role of CM in PHC services, enhance multi-disciplinary collaboration, and look into opportunities for further synergies with CM in PHC settings with a focus on chronic disease prevention and health management through promotion, health assessment, preventive care and introduction of new programmes with the involvement of CM. Relevant training programmes should also be devised for CMPs to foster mutual understanding of the PHC services provided by different healthcare professionals.
Recommendation 5.4
Enhance the role of allied health professionals and community pharmacists in the primary healthcare workforce
The Government sees the need to strengthen the role of other healthcare professionals in the local healthcare system, especially in PHC settings. We have already proposed to look into the regulatory restrictions on allied health professionals to enhance their functions and roles in the PHC workforce with a view to broadening the coverage of PHC services and enabling more professionals to assume PHC responsibilities.
In particular, we recommend to follow up with the statutory Boards and Councils of various healthcare professions on the recommendations in the Report of the Strategic Review on Healthcare Manpower Planning and Professional Development promulgated in 2017, including proposing legislative amendments to allow patients to have direct access to healthcare professional services (e.g. physiotherapy and occupational therapy) under specific circumstances, without a doctor’s referral.
Furthermore, to ensure the professional competency of healthcare personnel, we will legislate to make continuing professional education and/or CPD a mandatory requirement for supplementary medical professionals under the Supplementary Medical Professions Ordinance, as well as nurses and dentists. Drawing on the experience in implementing the on-going voluntary Accredited Registers Scheme for Healthcare Professions, we will also explore the feasibility of introducing a statutory registration regime for those healthcare professionals who are currently not subject to any statutory registration requirements such as clinical psychologists, speech therapists and dietitians, with a view to protecting public interest.
Primary Care Register
As recommended in paragraph 125, the Government proposes to develop sub-directories under the PCR for PTs, OTs and pharmacists in view of their extensive involvement in PHC for various medical conditions, in particular chronic illnesses and for long-term care. Sub-directories for other healthcare professionals (e.g. optometrists, nurses, speech therapists, dietitians, and other professionals who are not subject to any statutory registration requirements) shall also be developed in a later phase.
The inclusion of additional professions in the PCR shall help nurture a team approach and allow inter-disciplinary co-operation and cross-referral in a transparent, reliant manner. In addition, the quality of allied health professionals shall be assured through the enrolment and maintenance requirement imposed under the PCR.
Community Pharmacy
Pharmacists are becoming important providers of a wide range of healthcare services in the community to meet the needs of an ageing population and increasing number of people living with long-term health conditions. With active involvement of pharmacists, community pharmacy services also play an important role in PHC. Currently, pharmacists in DHCs are responsible for providing medication consultation to clients in order to maximise the benefit of drug treatment, reduce reliance and lower risk in the use of medicines. The pharmacists also work with other professionals of the multi-disciplinary team in health promotion and health education such as on medicine safety and smoking cessation.
During the COVID-19 pandemic, community pharmacies have offered to help refill HA patient prescriptions. To reduce the risk of infection and facilitate those patients under regular HA follow up who may not wish to visit HA’s clinics during the epidemic, patients are given an option to refill their medication through community pharmacies either by in-person pickup or home delivery. These community pharmacies also provide counselling service for patients in need. As the above drug dispensing model matures, it is proposed to regularise such model so as to enable designated community pharmacies to dispense drugs and provide drug counselling services to HA patients, especially those with stable conditions, as an alternative to frequenting clinics for follow up visits.
Table 5.3
- To recruit community pharmacists as part of the DHC network
- To strengthen pharmacists’ role by including them as part of the multi-disciplinary team in the care protocols of DHC’s structured chronic disease management programmes with a view to providing medication advice and counselling for DHC members, in particular those with polypharmacy, taking specific drugs (e.g. warfarin), newly diagnosed of diabetes mellitus /hypertension, discharged from hospital or having recent change of medication regime
- To utilise network community pharmacists in providing smoking cessation service for the public
- To provide other health promotion/disease prevention services as appropriate
- To further explore the role of community pharmacists in drug refill and related counselling in support of the public health system
To support the development of community pharmacy in Hong Kong, HHB has set up a Working Group on Community Pharmacy to advise on the following:
- development of community pharmacy services as steered by the SCPHD;
- enhancing training for pharmacists to support development of PHC; and
- defining the qualifications/training and work experience required for pharmacists to support programmes conducted by DHCs.
Against the above background, the Government proposes to enhance the role of community pharmacies, including supporting patients on monitoring of drug compliance, dispensing drugs to HA patients and patients joining the CDCC Scheme with a pre-defined community drug formulary.
Among others, drug costs have a significant contribution to healthcare expenditures, yet massive discrepancies in prices appear between different forms of drug purchases: between generic and patented drugs, and newly researched and older drugs [22]. The high recurrent drug expenditures for managing chronic diseases is one of the major factors driving patients to use public services. Alongside the CDCC Scheme, it is recommended to set up a community drug formulary composing mainly of generic drugs and selected patented drugs under which patients from the community could enjoy drugs at lower prices while receiving services from purchased primary care programmes in the private sector through the CDCC Scheme (see also Chapter 4- Recommendation 4.3).
Chapter 5 - REINFORCE PRIMARY HEALTHCARE MANPOWER Action Plan
5.1 PHC manpower Supply
To increase UGC-funded and subsidised healthcare training places
Action: Short
To invite Boards and Councils to increase the weighting of primary healthcare in their accreditation and placement programme
Action: Medium
To attract qualified non-locally trained PHC professionals to practise in Hong Kong
Action: Short
To reflect and refine the PHC manpower projection for healthcare professionals
Action: Short - Medium - Long
5.2 PHC Training
To continue to work with different institutions to provide PHC-related training courses
Action: Short
To strengthen professional training for family doctors, nurses, allied health professionals and social workers in PHC setting
Action: Medium
To establish a structured rotation system to facilitate the training of PHC professionals in different training settings in a co-ordinated manner
Action: Medium - Long
5.3 CMPs
To strengthen the role of CM in PHC settings
Action: Short - Medium - Long
To look into opportunities for further synergies with a focus on chronic disease prevention and health management
Action: Short - Medium - Long
To devise training programme for CMPs on PHC
Action: Medium
5.4 Allied Health Professionals and Community Pharmacists
To amend relevant Ordinances to allow patients’ direct access to certain healthcare professional services (e.g. physiotherapy and occupational therapy) under specific circumstances, without a doctor’s referral
Action: Short
To support the development of community pharmacy in Hong Kong under the advice of the Working Group on Community Pharmacy
Action: Short
To designate community pharmacies to dispense drugs
Action: Short - Medium
To engage community pharmacies to support the CDCC Scheme
Action: Short - Medium

