THE HEALTHCARE CHALLENGES IN HONG KONG
Ageing Population and Increase in Chronic Disease Prevalence
Hong Kong has one of the most rapidly ageing of population in the world and the speed of ageing will peak in the upcoming decade. The average annual increase rate of the population aged 65 and over will be 4.0% from 2021 to 2030. The population aged 65 and over will increase from 1.5 million (20% of the total population) in 2021 to 2.52 million (31% of the total population) in 2039. The proportion of old-old (aged 80 and over) will also rapidly increase from 0.4 million (5%) in 2021 to 0.93 million (11.5%) in 2039.
Ageing is also associated with increasing health and social care needs and higher prevalence of chronic diseases. The percentage of people who had chronic health conditions was 31% (around 2.2 million) in 2020/21, among which 47% were aged 65 and over. The number of Hospital Authority (HA) patients with chronic diseases is projected to reach 3 million in
the coming decade by 2039. More alarmingly, a substantial number of patients with chronic diseases – believed to be as many as a double of the diagnosed number – remain undiagnosed and unmanaged. Hypertension (HT) and diabetes mellitus (DM) are the highest in prevalence especially among the aged.
Chronic diseases are a major public health concern because of their impact on quality of life and productivity of the economy due to gradually deteriorating health conditions of the poorly managed patients, as well as their heavy burden to the public healthcare system in terms of high service utilisation and financial cost, especially when the associated complications are not timely intervened.
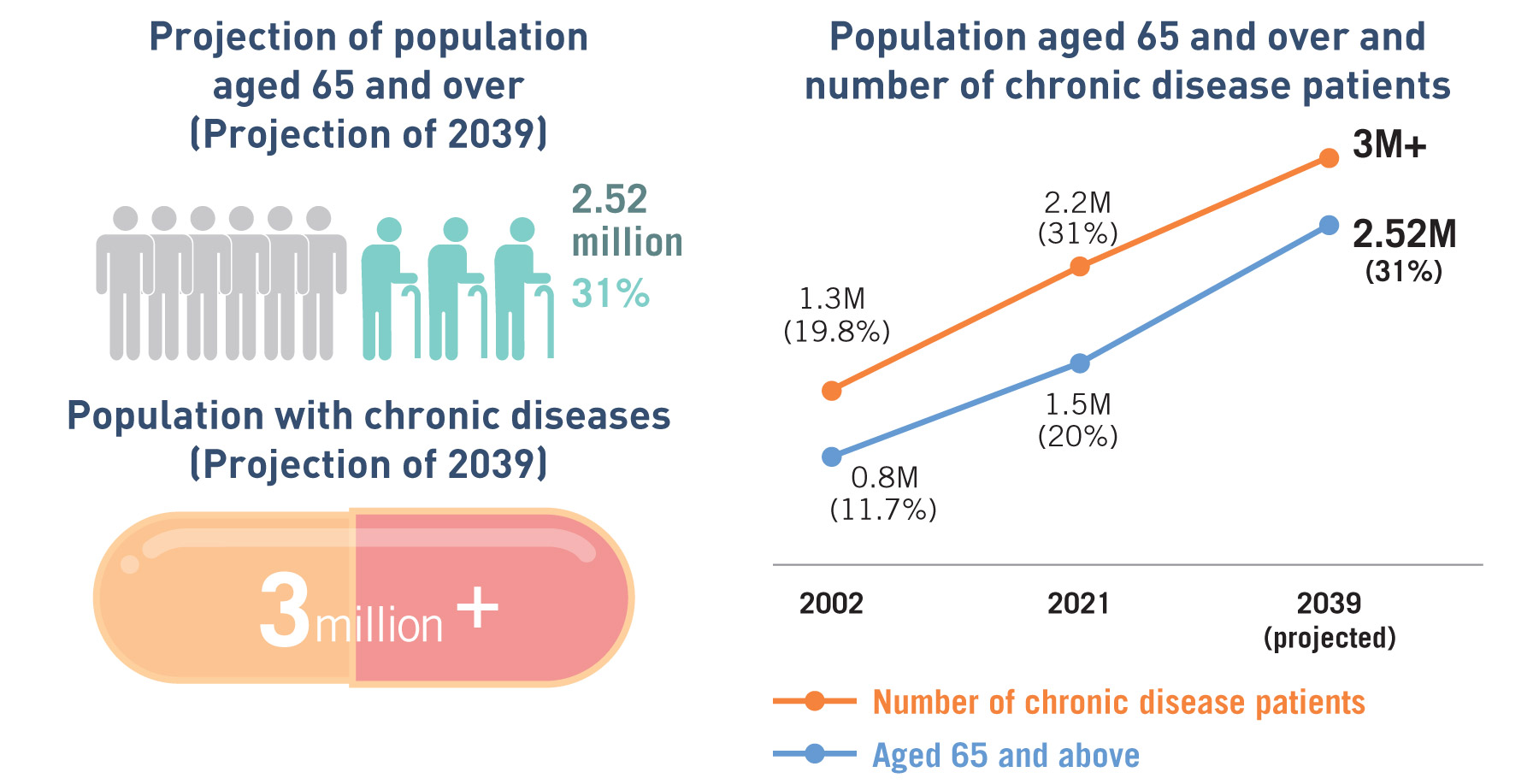
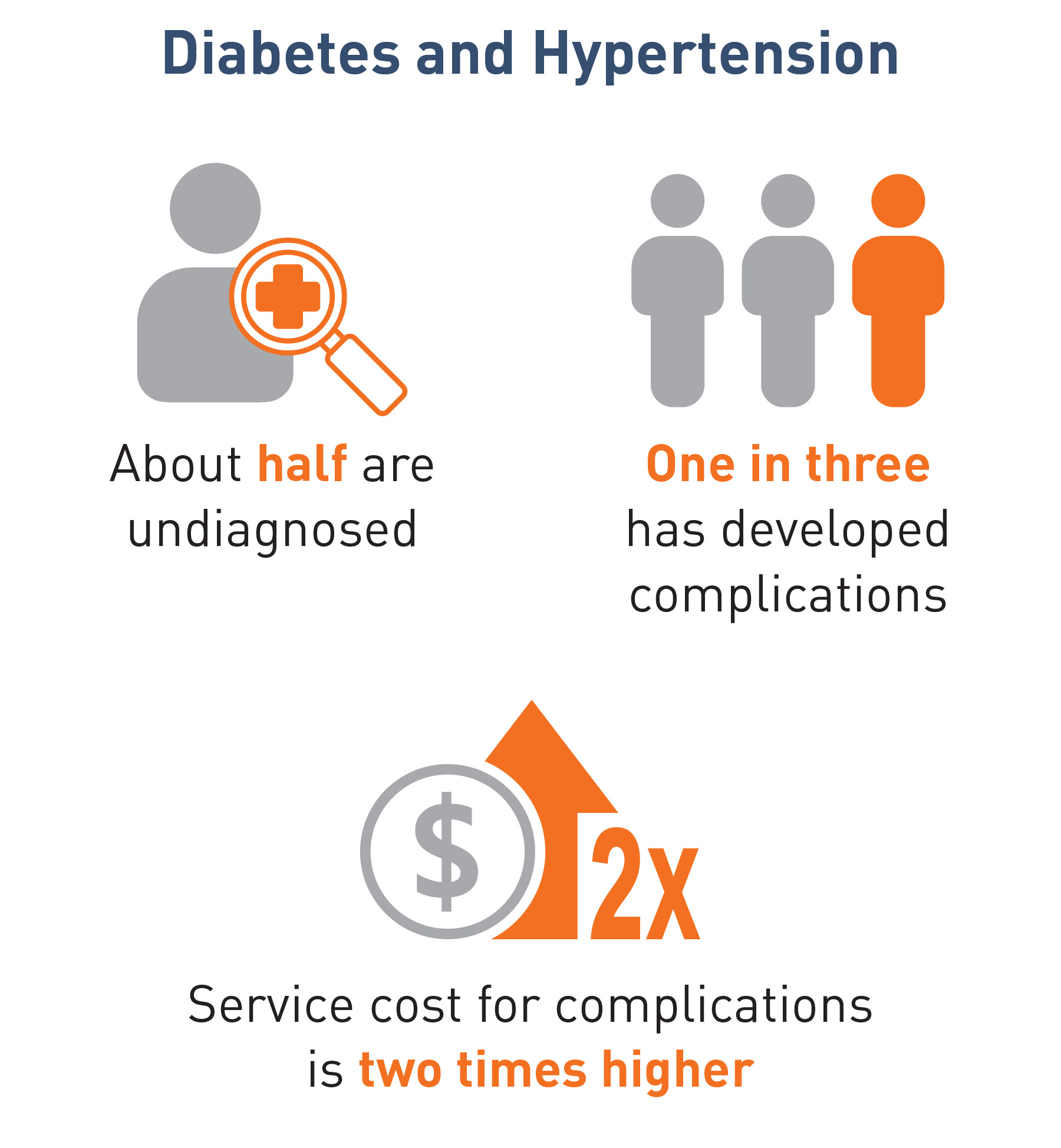
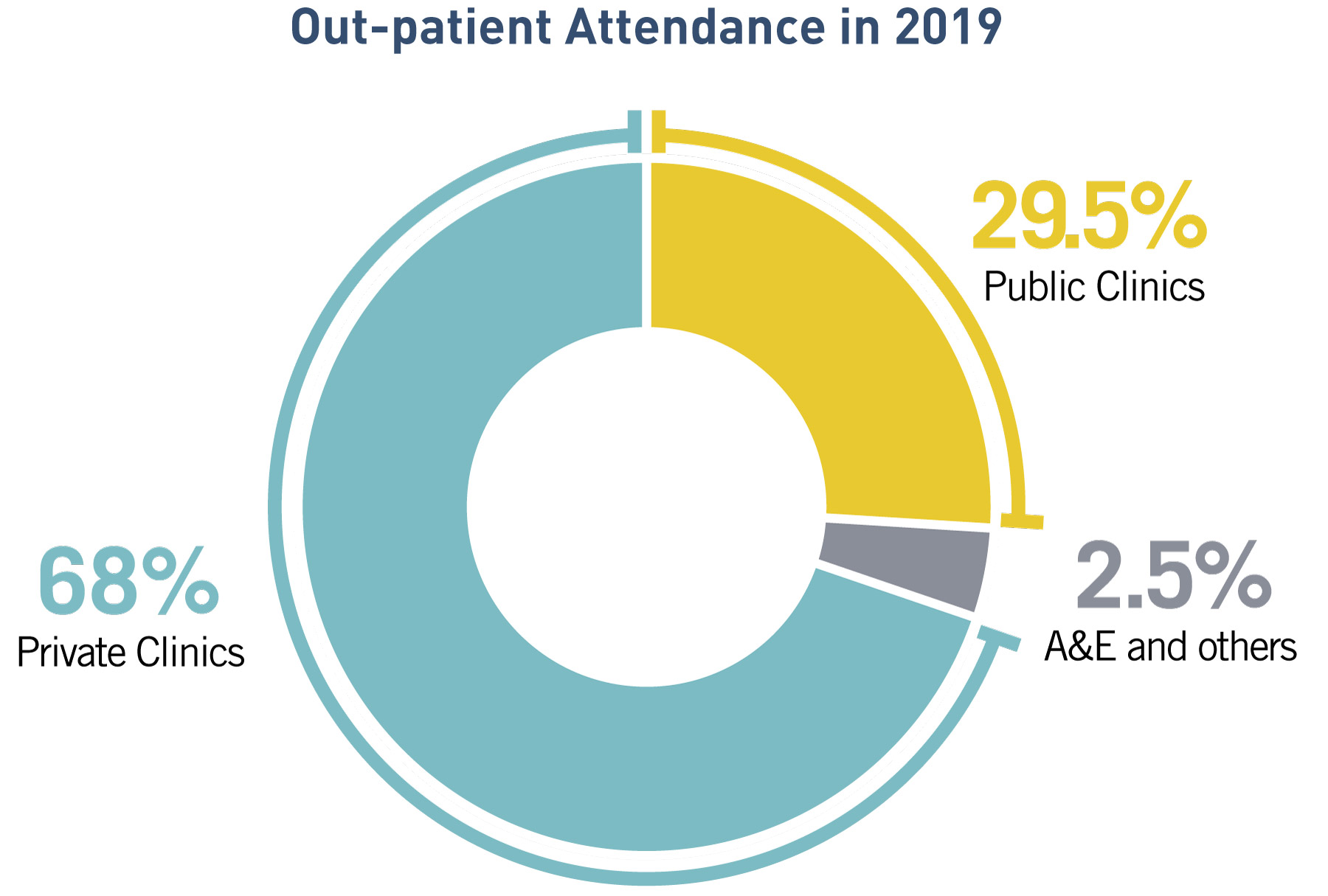
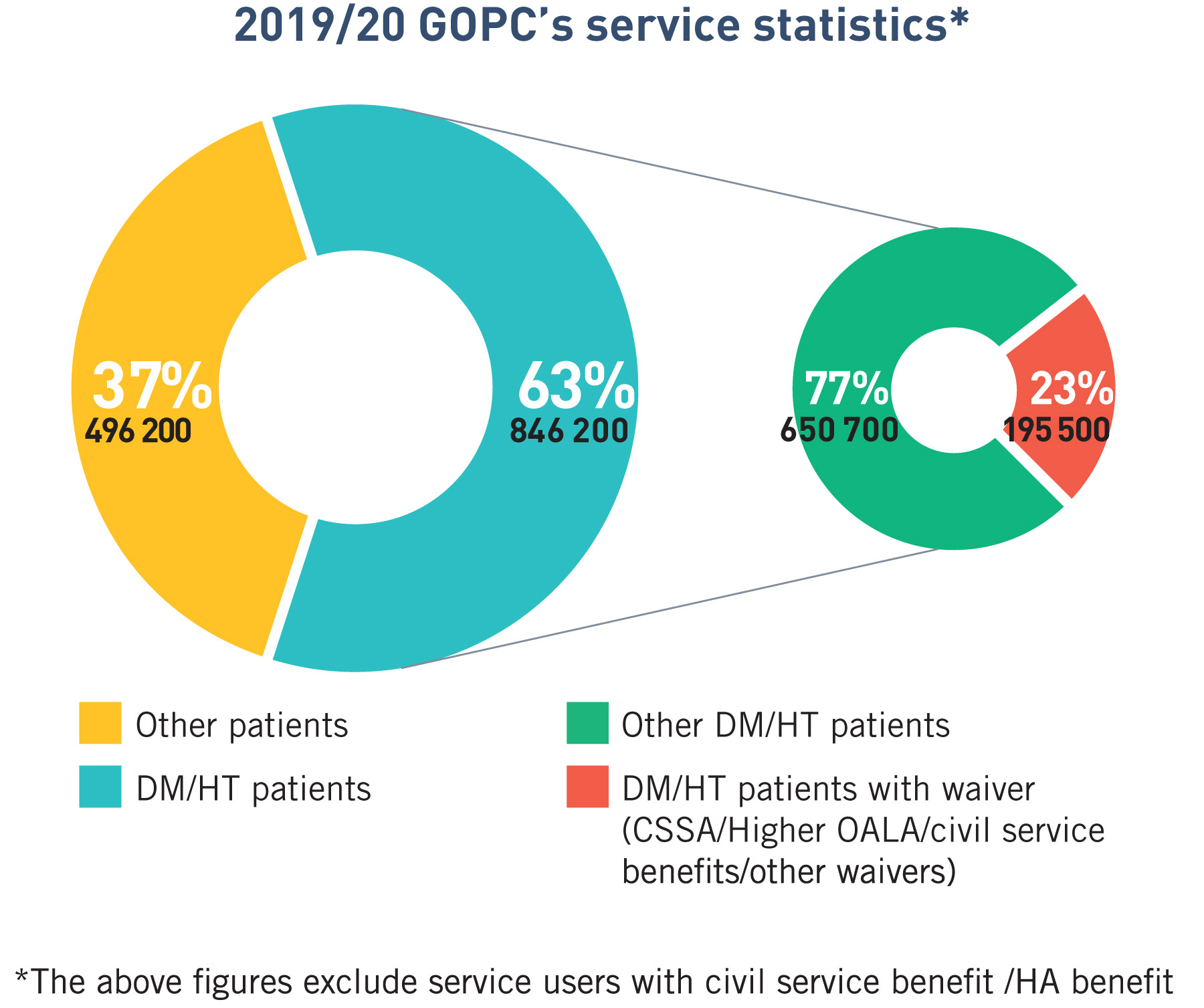
Ageing population and increasing chronic diseases prevalence is expected to exert a heavy toll on secondary/tertiary care especially the public hospitals. The utilisation rate of hospital service rises exponentially for people aged 65 and over. Despite only making up 18% of the population, they accounted around half of all patient days and Accident and Emergency (A&E) admissions and over one-third of General Out-patient Clinic (GOPC) and Specialist Out-patient Clinic (SOPC) attendances in 2019. Among GOPC, Family Medicine Specialist Clinic and SOPC patients, around 60% have selected chronic diseases, of which 82% have DM/HT. According to HA, among DM/HT patients, one in three has developed complications in 2019, and their per capita service cost was two times higher than those without complications.
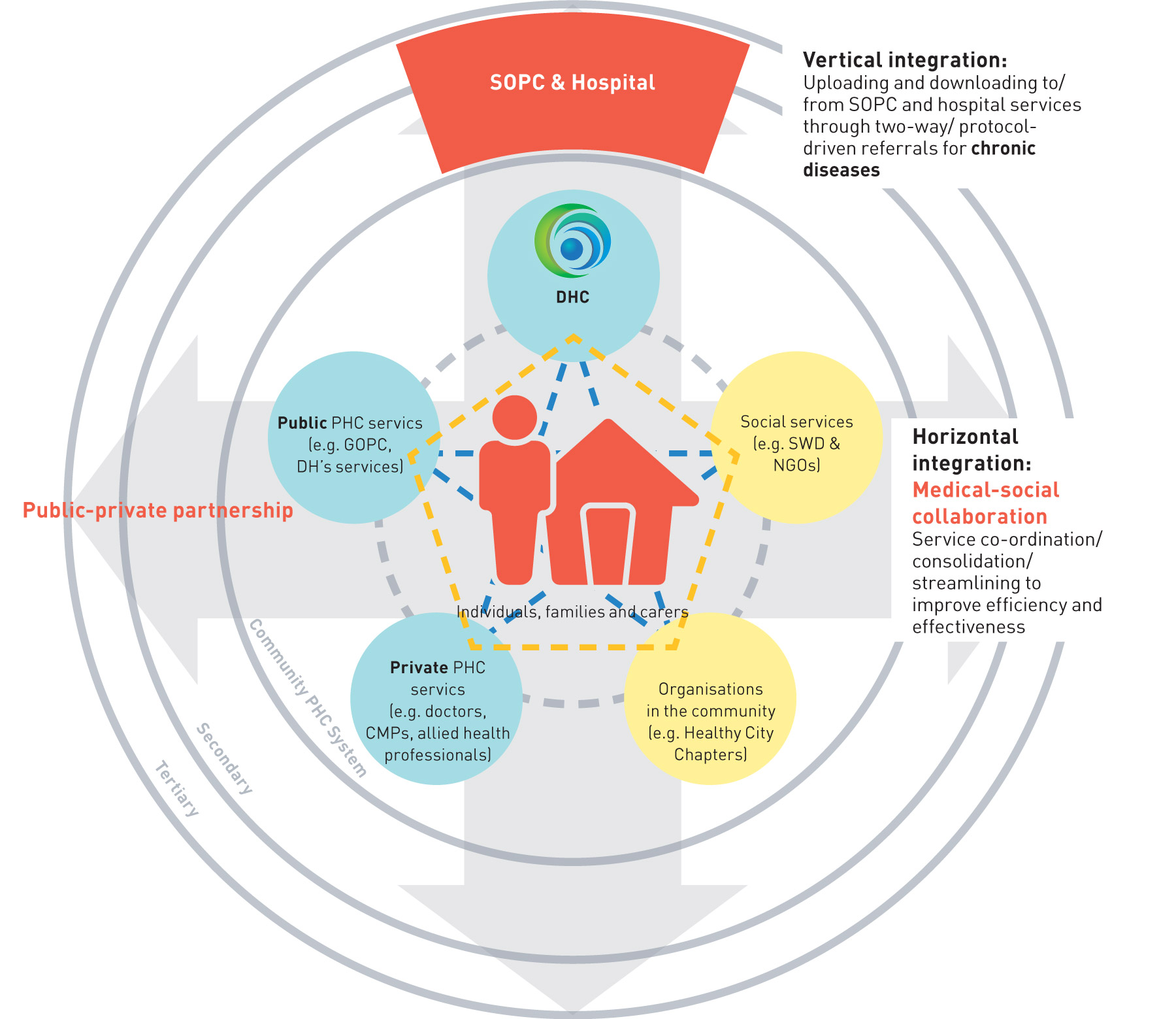
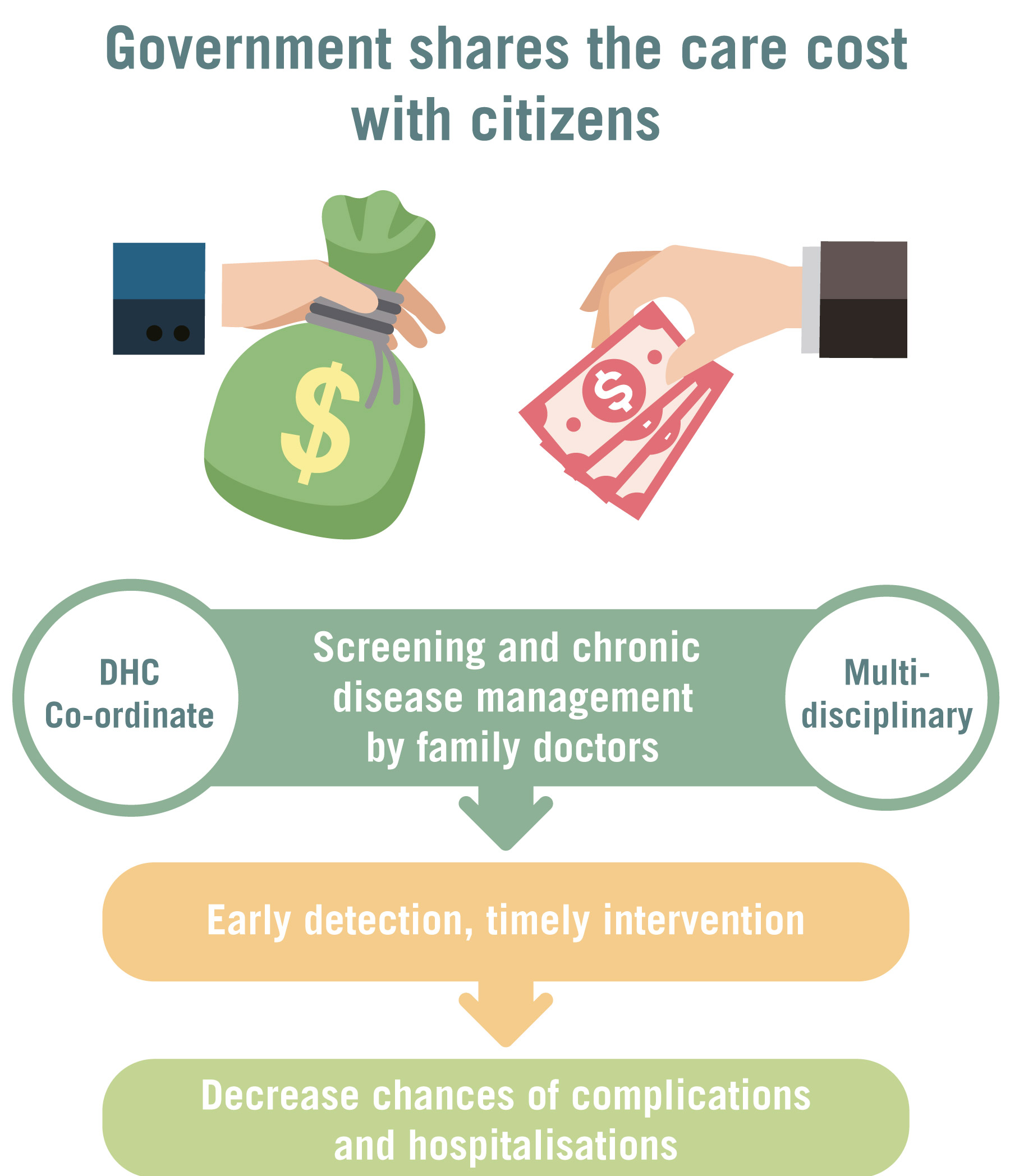
To achieve better population health and quality of life, we need to shift the centre of gravity of our healthcare system from treatment-oriented institution-centric secondary/tertiary healthcare to prevention-oriented, family-centric PHC. Through well-managed and co-ordinated healthcare at the community level, we envisage that chronic disease patients’ medical and health needs will be properly taken care of at the community level. In turn, alongside longevity, their physical well-being and quality of lives will be enhanced, their morbidity will be compressed and their needs for hospital care will be reduced and deferred. The overall health status of the population shall thereby be improved.
Health system sustainability
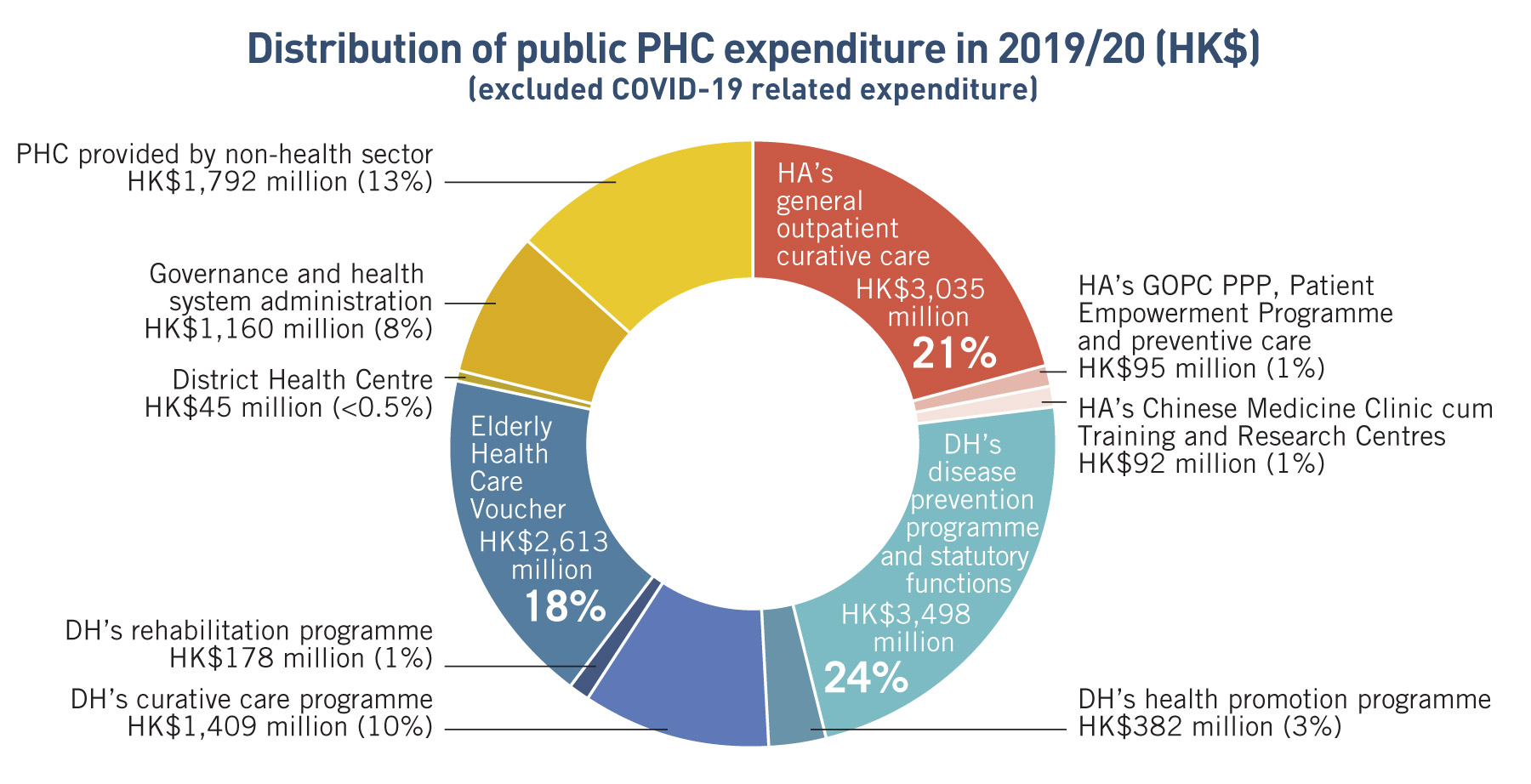
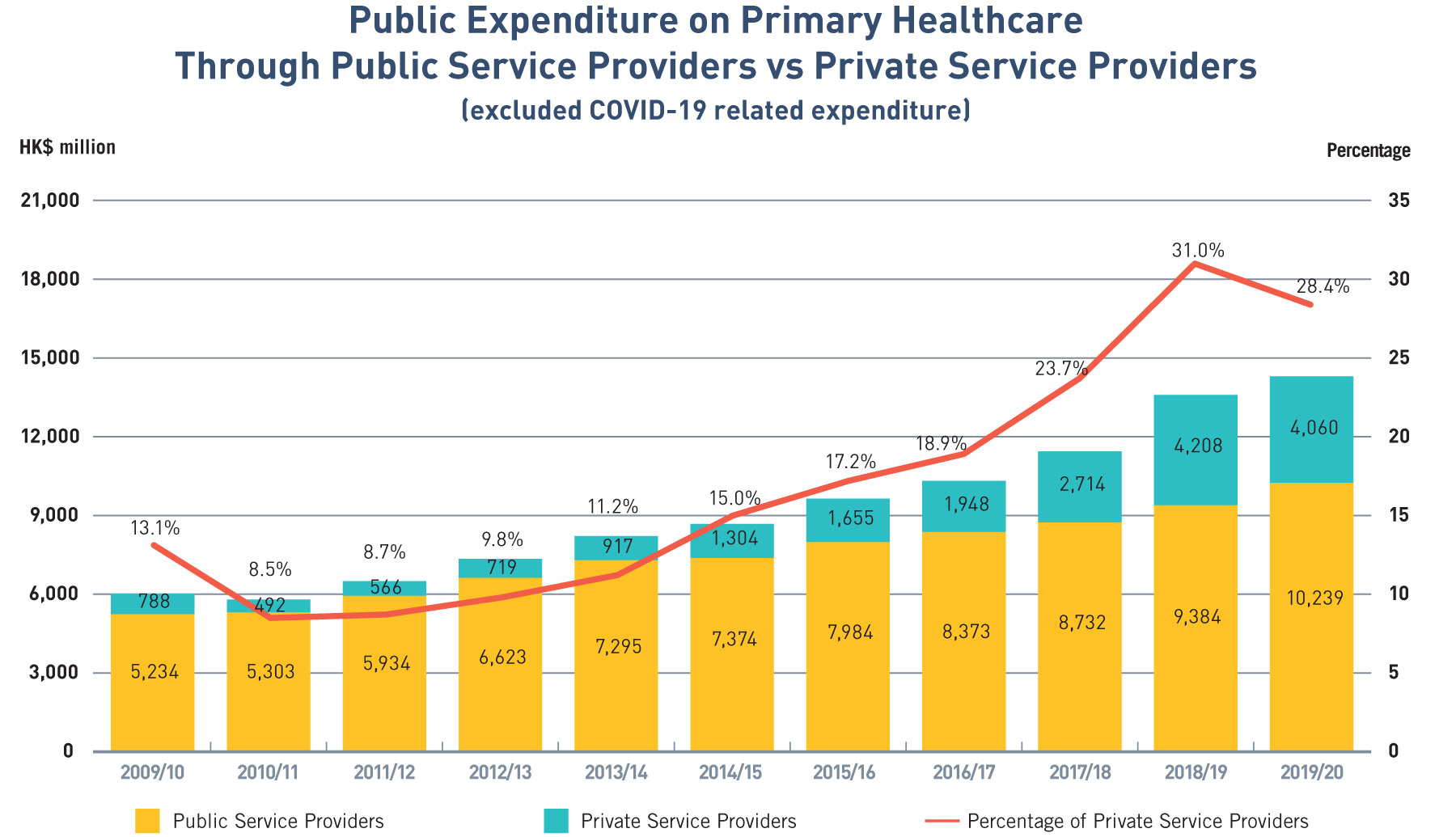
Currently, treatment-oriented secondary and tertiary healthcare especially public hospital services accounted for the majority of healthcare services and spending in Hong Kong. According to the Domestic Health Accounts (DHA) in 2019/20, the total current health expenditure in Hong Kong is roughly split at 30:70 between PHC ($52.9 billion) and secondary/tertiary healthcare ($127.3 billion). Owing to heavily subsidised public hospital services (at over 97% of costs), public healthcare expenditure is even more concentrated with around 83% ($79.9 billion) of public health expenditure spent on secondary and tertiary healthcare whereas only 17% was spent on PHC ($16.0 billion).
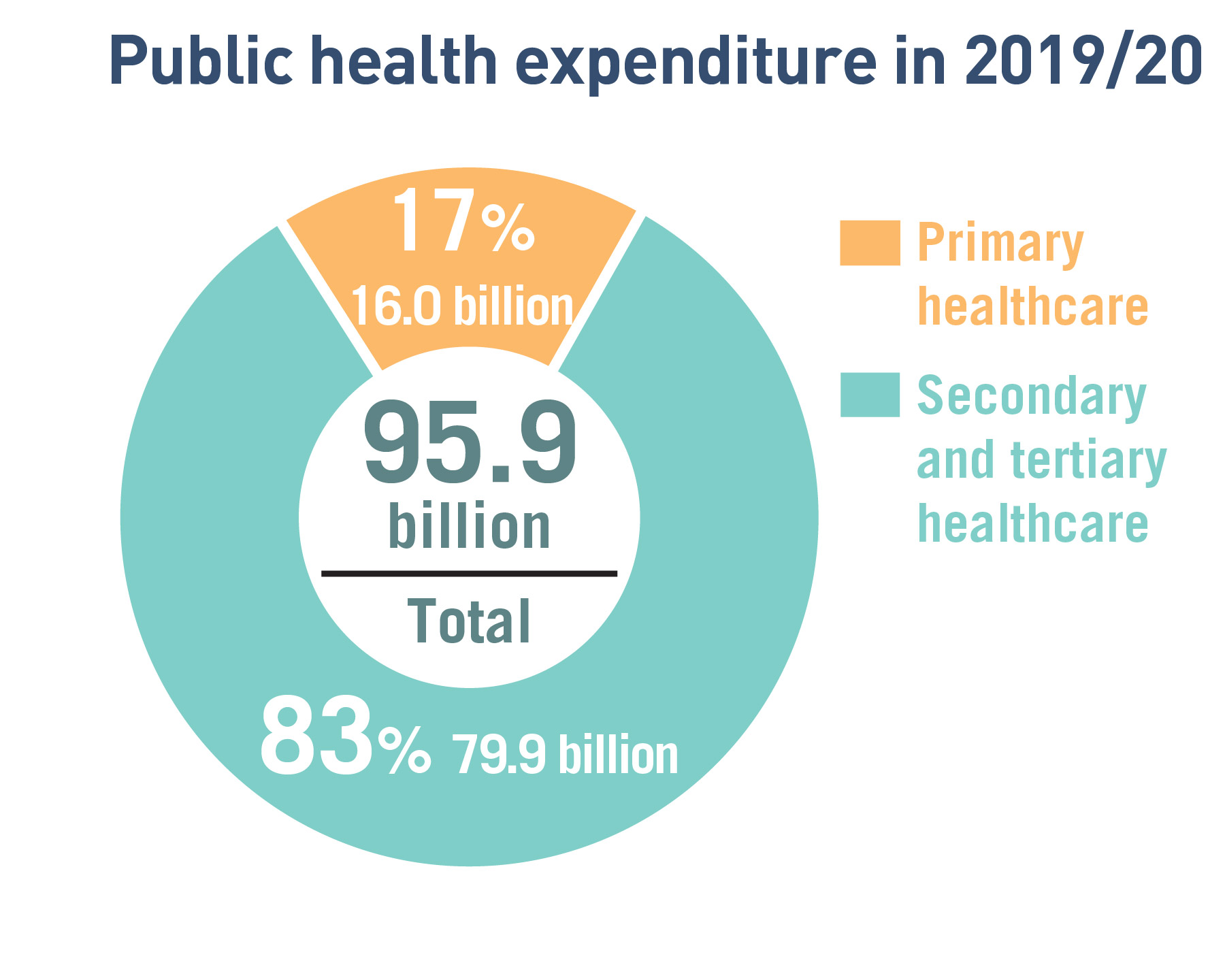
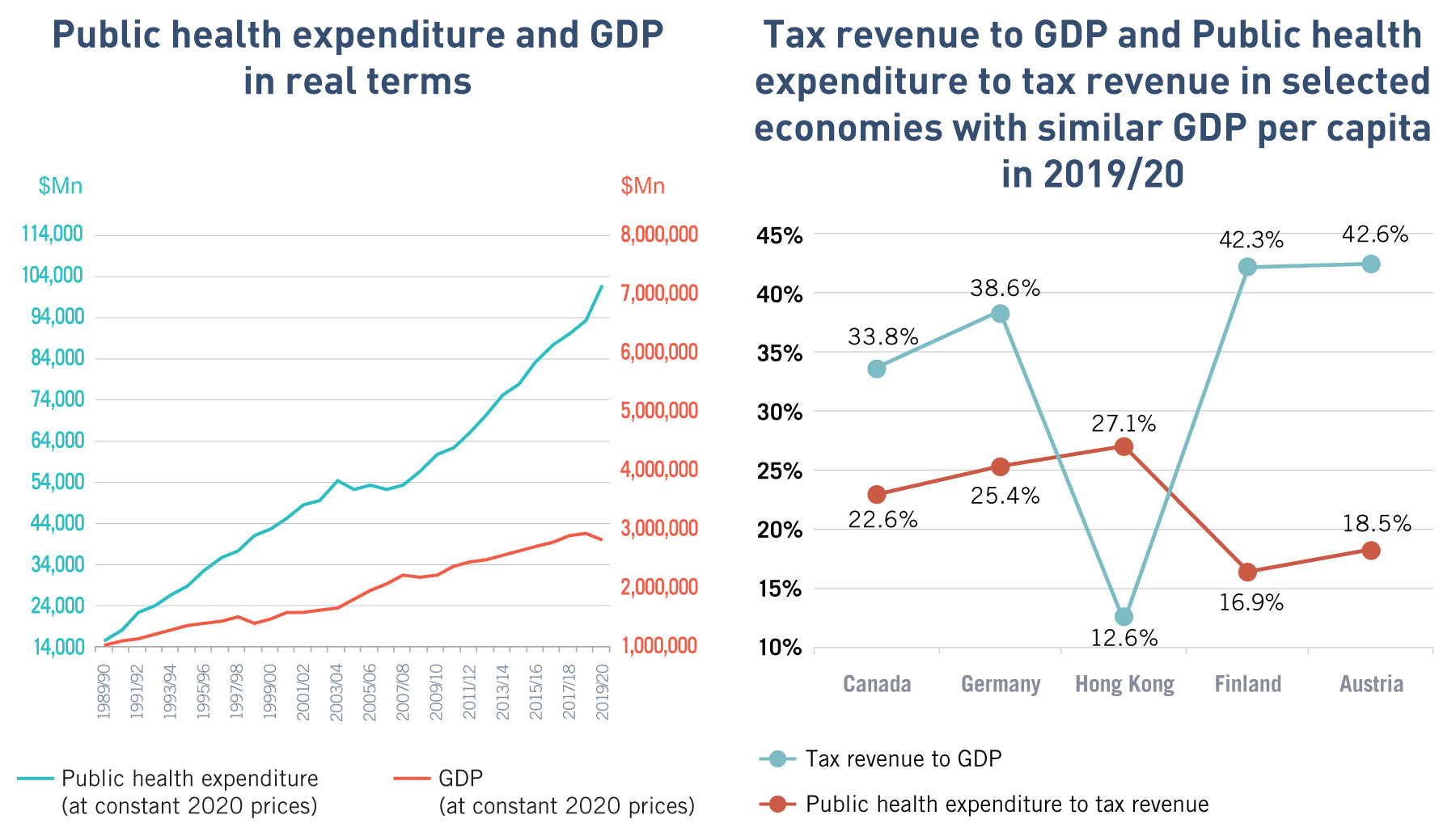
Treatment-oriented healthcare induces higher healthcare costs and accelerates the increase of health expenditure. From 2010/11 to 2019/20, our average annual growth rate of public health expenditure was 5.6%, faster than that of GDP at 2.0% in real terms. According to the projection based on a research commissioned by the then Food and Health Bureau in 2008, it was estimated that total/public healthcare expenditure would increase from 5.3%/2.9% of GDP in 2004 to 7.1%/4.1% of GDP in 2020 if nothing was done to reform the healthcare system. Actual total/public healthcare expenditure (excluding COVID-19 expenditure) was estimated to be about 6.7%/3.6% of GDP in 2019/20, illustrating that various reforms over the years might have helped to curb the expenditure increase.
Having said that, the accelerating ageing of the population in the coming decade will on one hand further limit GDP growth and the budget for public health expenditure, and on the other hand increase the demand for public health spending. It is simply unsustainable to keep increasing public health expenditure to fund the public hospital system to cope with the ever-increasing healthcare demand, unless systemic reform to the healthcare system is introduced.

Publicly-funded primary healthcare services
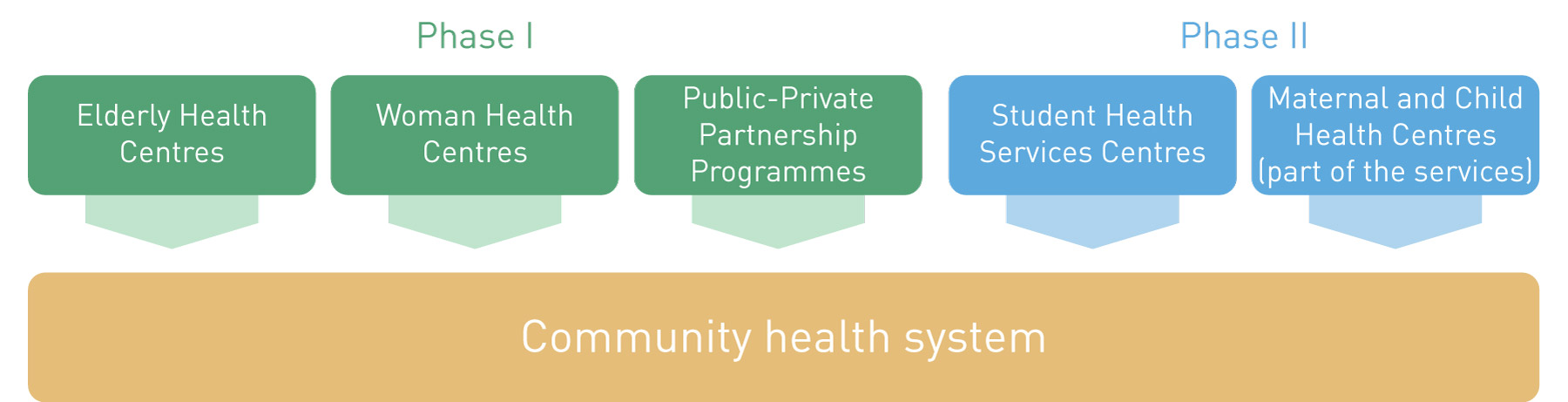
Over the years, the Government has been providing publicly-funded PHC mainly through direct services of the Department of Health (DH) and HA. In recent years, the Government has launched various government-subsidised or public-private partnership (PPP) healthcare programmes as recommended in previous healthcare reform consultation documents with a view to tapping into the private healthcare sector resources in meeting the demand for public PHC service and enhancing the quality of health of the population. These include the Vaccination Subsidy Scheme since 2008, Elderly Health Care Voucher (EHCV) Scheme since 2009, General Out-Patient Clinic PPP Scheme since 2014, and Colorectal Cancer Screening Programme since 2016. Together these subsidised programmes accounted for some 3 billion government fixed expenditure on PHC in 2019/20.

Since 2019, the Government is committed to enhancing district-based PHC services by setting up DHCs throughout the territory progressively, with a view to strengthening collaboration between the health and social care sectors and public-private partnership in a district setting, enhancing public awareness in disease prevention and self-health management, offering greater support for patients with chronic diseases, and relieving the pressure on specialist and hospital services. Operated by a non-government entity through government funding, the DHC is a brand new service model and will be a key component of the PHC system in a bid to shift the emphasis of the present healthcare system and people’s mindset from treatment-oriented to prevention-oriented.
To build up a critical mass of district-based PHC services throughout the territory, the Government has set up DHCs (and DHC Expresses of smaller scale in the interim) in all districts across the territory by 2022. DHCs will progressively strengthen their role as the co-ordinator of community PHC services and case manager to support PHC doctors on one hand, and their role as district healthcare services and resource hub that connect the public and private services provided by different sectors in the community on the other hand, thereby redefining the relationship among public and private healthcare services; as well as PHC and social service providers.

Private primary healthcare providers and public-private partnership
To improve accessibility to quality PHC for the general public and redress the imbalance between the public and private healthcare sector, strategically the Government strives to optimise the utilisation of private healthcare resources and leverage on the private sector’s capacity for providing PHC services, with a view to relieving pressure on the public sector and thereby enhancing the sustainability of the healthcare system. As recommended in the “Your Health Your Life” healthcare reform consultation document in 2008, PPP in healthcare should be pursued in Hong Kong to subsidise the community to make better use of resources in the private sector to deliver service for some public sector patients, thus allowing the public healthcare system to continue to serve as an essential safety net for the population and be accessible to those who lak the means to pay.
In doing so, there is a need for standardisation and assurance of the quality of PHC services across public and private service providers to ensure that the whole PHC system is driving towards the Government’s overall PHC policy and delivering the intended health outcomes. Enhancement of performance monitoring tools, improvement on standardisation and transparency in the private PHC sector to unleash their potential in achieving continuity of care, care co-ordination and gate-keeping are some of the key issues to be addressed. With the participation of well-managed private PHC providers in the PHC system, we envisage to see improvements in the quality of health for individuals and the population as a whole.
OUR VISION FOR THE PRIMARY HEALTHCARE SYSTEM
The Direction of Primary Healthcare Reform
1. Develop a Community-based Primary Healthcare System
Challenges and our aims
Recommendations
- To progressively migrate PHC services under DH to the district-based community health system, especially those with room for more efficient delivery through an alternative approach, with a view to facilitating provision of integrated PHC services through the district-based community health system and reducing service duplication.
2. Strengthen Primary Healthcare Governance
Challenges and our aims
Recommendations
To strengthen PHC governance, we propose the following –
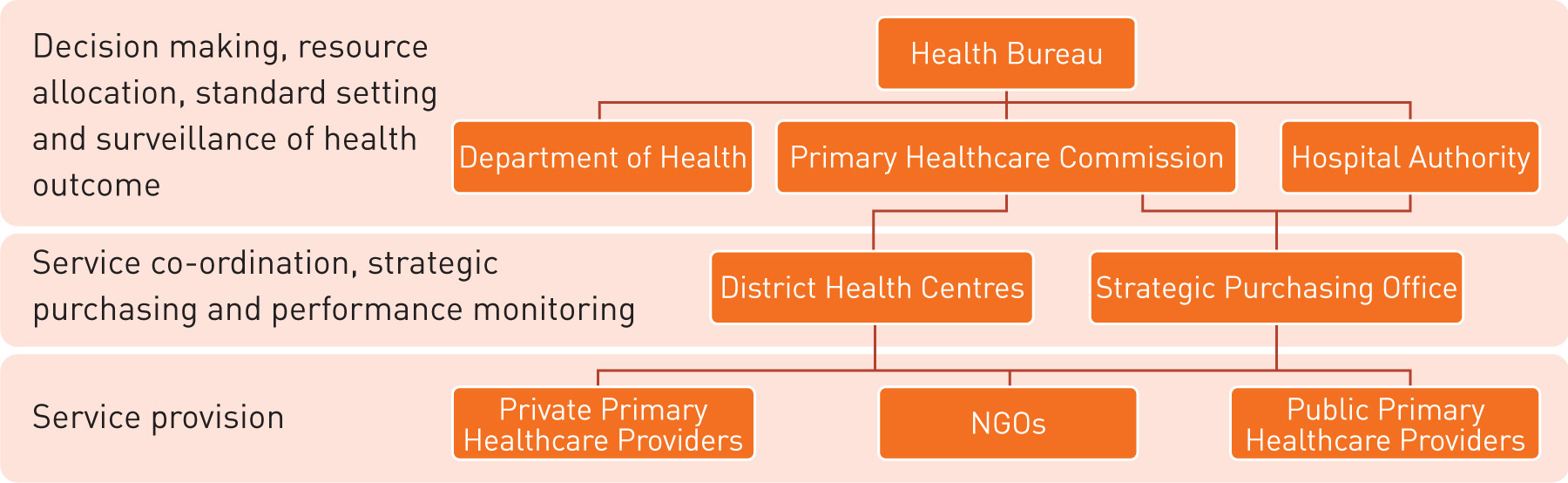
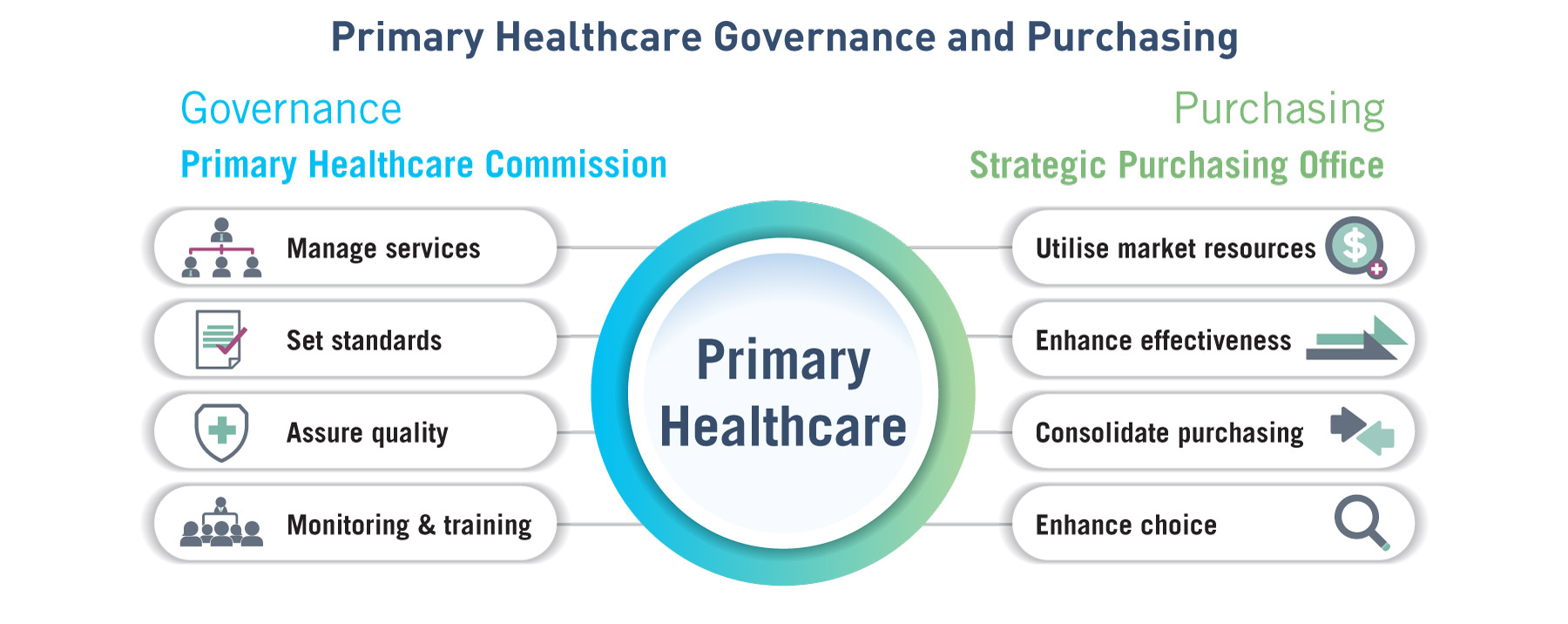
- To progressively transform the Primary Healthcare Office currently under the Health Bureau into the Primary Healthcare Commission empowered to oversee PHC service delivery, standard setting, quality assurance and training of PHC professionals under one roof, as well as to take on PHC service planning and resource allocation through strategic purchasing supported by the Strategic Purchasing Office.
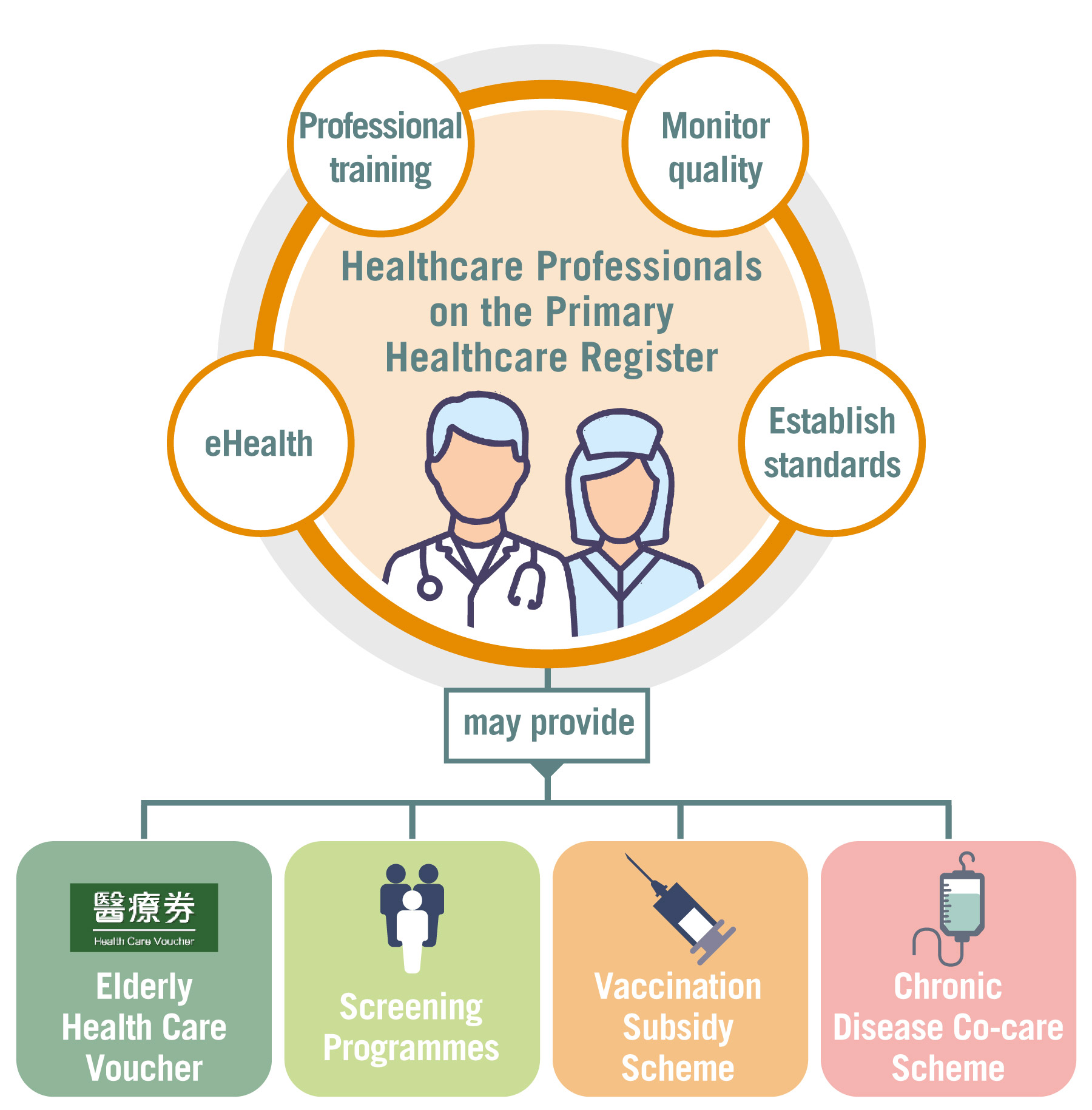
- To require all family doctors and healthcare professionals participating in PHC service provision to be enlisted on the Primary Care Register and commit to using the PHC reference frameworks, including those enrolling in government-subsidised programmes such as the EHCV Scheme and various PHC PPP Programmes such as CDCC Scheme, in order to ensure the quality of PHC services, establish the “gold standard” for PHC service providers, and provide incentives for PHC professionals to participate in multi-disciplinary PHC services and adopt best practices.
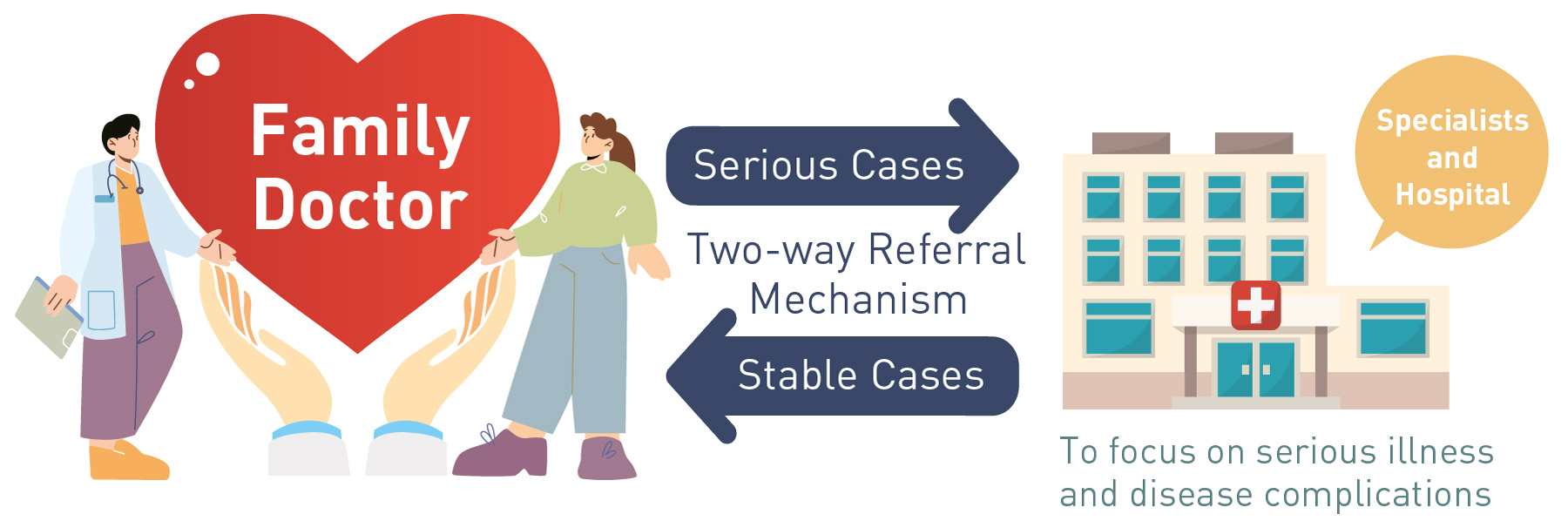
- To establish the two-way referral mechanism between PHC services in both the public and private sectors with the specialist and hospital services, emphasising the effective discharge of case management and gate-keeping role of PHC service providers, allowing timely and appropriate referral of patients with complications by primary care doctors to specialists and public hospitals for secondary care, and allowing continuing follow-up, monitoring and disease management of patients in stable conditions by primary care doctors.
3. Consolidate Primary Healthcare Resources
Challenges and our aims
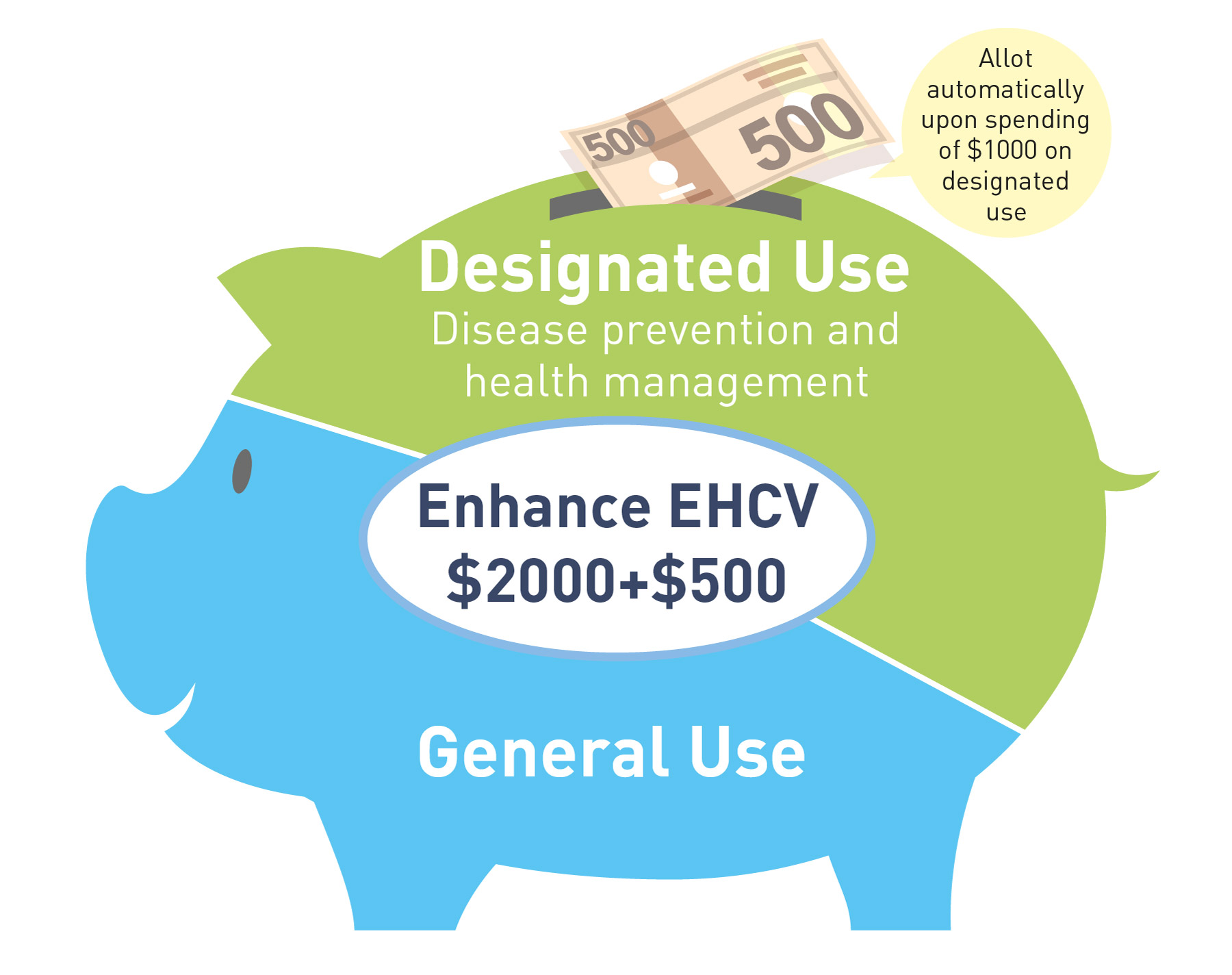
- To improve EHCV Scheme to direct resources towards PHC services with an emphasis on strengthening chronic disease management and reinforcing the different levels of prevention, by incentivising elders to use EHCVs for continuous preventive healthcare and chronic disease management with healthcare service providers registered under the Primary Care Register, such as health assessment, chronic disease screening and management or other government initiatives.
- To establish a Strategic Purchasing Office under Health Bureau to oversee the development and implementation of strategic purchasing programmes at primary care level, so as to channel resources more effectively towards quality, co-ordinated and continuous PHC with an emphasis on prevention-oriented, community-based and family-centric services, reduce service duplications, gaps, inefficiencies and mismatches between the public and private sectors in PHC, and ultimately bring about optimised co-ordinated and integrated care to individuals and families to maximise their health benefits and outcomes.
4. Reinforce Primary Healthcare Manpower
Challenges and our aims
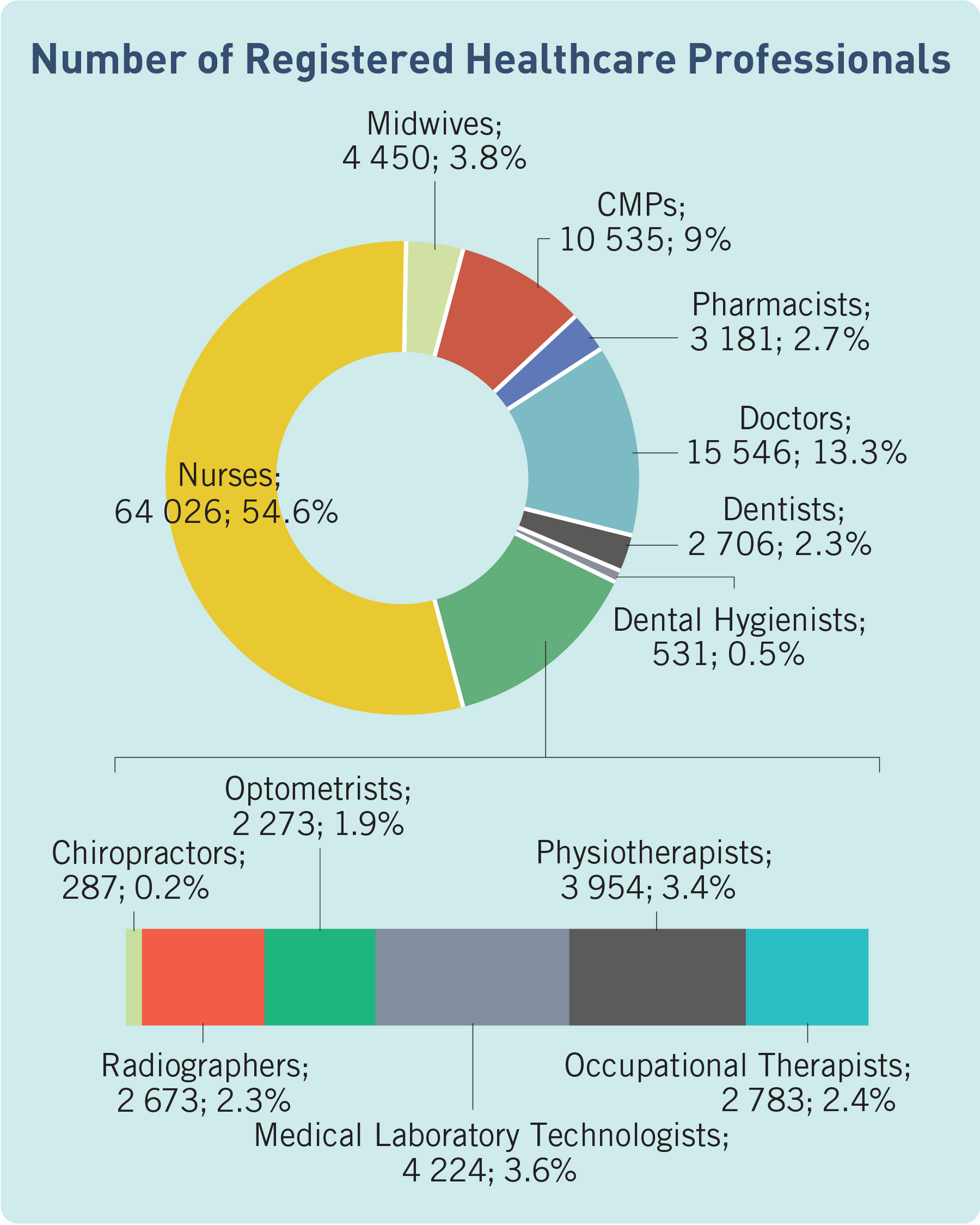
The sustained delivery of quality and adequate PHC services relies on the stable and sufficient supply of qualified PHC manpower with sufficient knowledge, skills and attitude, who embraces the concept of multi-disciplinary teamwork and specialises in the team setting in PHC in the community. The training of PHC professionals and enhancing the role of PHC professionals are therefore essential to ensure adequate quantity and quality of manpower supply.
Recommendations
5. Improve Data Connectivity and Health Surveillance
Challenges and our aims
Recommendations
- To develop a population-based health dataset and conduct on-going data analytics and surveys, and commission research studies on population-based health status, disease pattern and burden, and health seeking pattern, etc., with a view to providing the necessary data, evidence and analysis to support health policy making by the Government, PHC service planning and resource allocation by the Primary Healthcare Commission as well as the corresponding service planning and resource allocation for the public hospital system.